
| Size | Price | Stock | Qty |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|
Purity: ≥98%
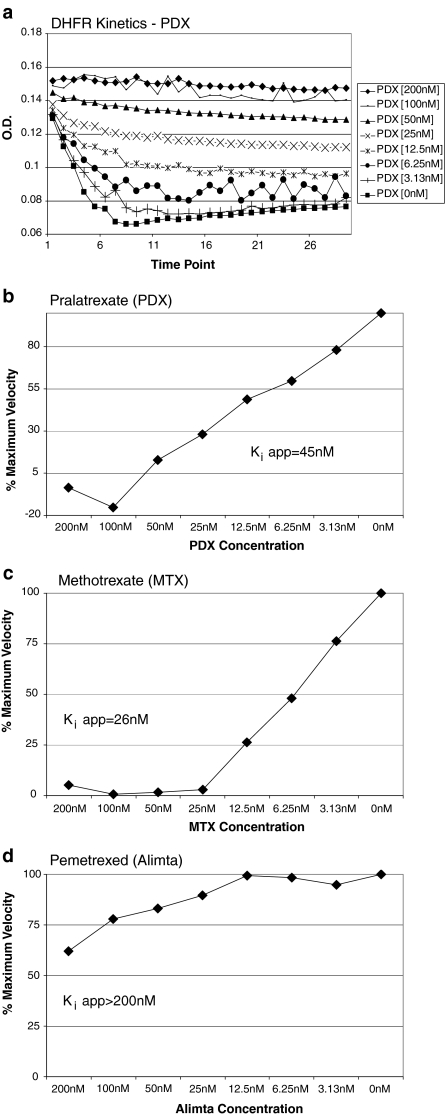
Pralatrexate (PDX; trade name Folotyn), an antifolate which is structurally a folate analog, is a potent and selective inhibitor of dihydrofolate reductase (DHFR) exhibiting high affinity for reduced folate carrier-1 (RFC-1) with antineoplastic and immunosuppressive activities. Pralatrexate has been approved by FDA to treat a certain type of cancer called peripheral T-Cell lymphoma-PTCL.
| ln Vitro |
When administered to different T lymphoma cell lines, pralatrexate (100 pM-200 μM; 48-72 h) demonstrates cytotoxicity that is dependent on both concentration and time. The following are the IC50 values at 48 and 72 hours: 1.1 and 2.5 nM for H9 cells; 1.7 and 2.4 nM for P12 cells; 3.2 and 4.2 nM for CEM cells; 5.5 and 2.7 nM for PF-382 cells; 1 and 1.7 nM for KOPT-K1 cells; 97.4 and 1.2 nM for DND-41 cells; and 247.8 nM and 0.77 nM for HPB-ALL cells. After 48 hours of treatment, HH cells showed some resistance, with an IC50 of 2.8 nM at 72 hours [1]. Treatment with pralidoxate (2-5.5 nM; 48-72 h; H9, HH, P12, and PF382 cells) results in strong apoptosis and caspase-8 and caspase-9 activation [1]. Treatment of H9 and P12 cells with pralitrexate (3 nM; 16–48 hours) dramatically raises p27 levels and promotes the accumulation of inducible folate carrier type 1 (RFC-1) in the cells [1].
|
|---|---|
| ln Vivo |
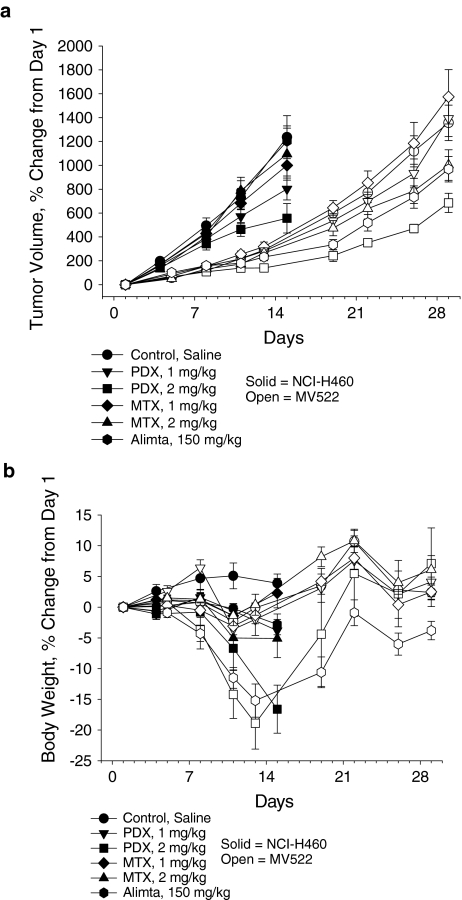
In comparison to either drug alone, the combination of Bortezomib (0.5 mg/kg) and Pralatrexate (15 mg/kg; intraperitoneal injection; on days 1, 4, 8, and 11; SCID-beige mice) increased effectiveness [1].
|
| Cell Assay |
Cell Cytotoxicity Assay[1]
Cell Types: T-lymphoma cell lines Tested Concentrations: 100 pM-200 µM Incubation Duration: 48 hrs (hours), 72 hrs (hours) Experimental Results: demonstrated concentration- and time-dependent cytotoxicity against a broad panel of T-lymphoma cell lines. Apoptosis Analysis[1] Cell Types: H9, HH, P12 and PF382 cells Tested Concentrations: 2 nM, 3 nM, 4 nM, 5.5 nM Incubation Duration: 48 hrs (hours), 72 hrs (hours) Experimental Results: Induced potent apoptosis and caspase activation. Western Blot Analysis[1] Cell Types: H9 and P12 cells Tested Concentrations: 3 nM Incubation Duration: 16 hrs (hours), 24 hrs (hours), 48 hrs (hours) Experimental Results: Clearly increased p27 levels and increased the accumulation of RFC-1 in cells. |
| Animal Protocol |
Animal/Disease Models: SCID-beige mice (5-7weeks old) injected with HH cells[1]
Doses: 15 mg/kg Route of Administration: intraperitoneal (ip)injection; on days 1, 4, 8, and 11 Experimental Results: demonstrated superior efficacy in T-cell malignancies. |
| ADME/Pharmacokinetics |
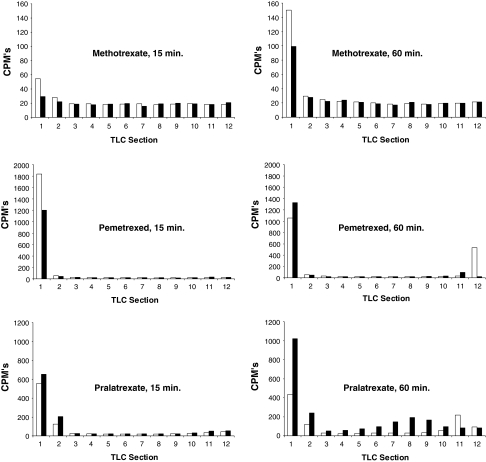
Absorption, Distribution and Excretion
With an intravenous formulation, pralatrexate has complete bioavailability. Pralatrexate demonstrates a dose-proportional and linear pharmacokinetics over a dose range of 30-325 mg/m2. Upon an intravenous push over 3 to 5 minutes of a starting dose of 30 mg/m2 racemic pralatrexate for dose 1 of cycle 1, Cmax and AUC0-∞ was estimated to be 5,815 ng/mL and 267,854 ng/mL.min respectively using a noncomparmental pharmacokinetics analysis.Both pralatrexate diastereomers demonstrates a multiphase decline in plasma concentration with a rapid initial fall followed by a slow terminal phase. The initial fall is thought to reflect the clearance of pralatrexate by renal and non-renal mechanism , while the slow terminal phase likely represents the return of pralatrexate from deep intracellular compartments, enterohepatic circulation, or after deglutamination. Following a single dose of FOLOTYN 30 mg/m2, approximately 34% of the pralatrexate dose was excreted unchanged into urine. Following a radiolabeled pralatrexate dose, 39% (CV = 28%) of the dose was recovered in urine as unchanged pralatrexate and 34% (CV = 88%) in feces as unchanged pralatrexate and/or any metabolites. 10% (CV = 95%) of the dose was exhaled over 24 hours. The steady-state volume of distribution of pralatrexate S- and R-diastereomers is 105 L and 37 L, respectively. The total systemic clearance of pralatrexate diastereomers was 417 mL/min (S-diastereomer) and 191 mL/min (R-diastereomer). The pharmacokinetics of pralatrexate administered as a single agent at a dose of 30 mg/sq m administered as an intravenous push over 3-5 minutes once weekly for 6 weeks in 7-week cycles have been evaluated in 10 patients with PTCL. The total systemic clearance of pralatrexate diastereomers was 417 mL/min (S-diastereomer) and 191 mL/min (R-diastereomer). Pralatrexate total systemic exposure (AUC) and maximum plasma concentration (Cmax) increased proportionally with dose (dose range 30-325 mg/sq m, including pharmacokinetics data from high dose solid tumor clinical studies). The pharmacokinetics of pralatrexate did not change significantly over multiple treatment cycles, and no accumulation of pralatrexate was observed. Pralatrexate diastereomers showed a steady-state volume of distribution of 105 L (S-diastereomer) and 37 L (R-diastereomer). In vitro studies indicate that pralatrexate is approximately 67% bound to plasma proteins. For more Absorption, Distribution and Excretion (Complete) data for Pralatrexate (7 total), please visit the HSDB record page. Metabolism / Metabolites While the liver has been shown to metabolize pralatrexate to some extent, pralatrexate is not significantly metabolized by any CYP450 isozymes or glucuronidases in vitro. In vitro studies using human hepatocytes, liver microsomes and S9 fractions, and recombinant human CYP450 isozymes showed that pralatrexate is not significantly metabolized by the phase I hepatic CYP450 isozymes or phase II hepatic glucuronidases. Biological Half-Life The terminal elimination half-life of pralatrexate was 12-18 hours (coefficient of variance [CV] = 62-120%). The terminal elimination half-life of pralatrexate was 12-18 hours (coefficient of variance (CV) = 62-120%). |
| Toxicity/Toxicokinetics |
Hepatotoxicity
Pralatrexate is associated with serum enzyme elevations during therapy, but these abnormalities are generally mild and self-limited, rising to above 5 times ULN in 2% to 6% of patients and rarely requiring dose adjustment. No instances of clinically apparent acute liver injury attributed to pralatrexate have been reported in the literature, but monitoring for liver toxicity is recommended. Pralatrexate has not been linked specifically to sinusoidal obstruction syndrome, but it is rarely used in high doses in neoplastic disease or in conditioning regimens for bone marrow transplantation, situations in which alkylating agents are commonly associated with this complication. Likelihood score: E* (unlikely but suspected rare cause of liver injury). Protein Binding The protein binding of pralatrexate is approximately 67% in vitro. Interactions The effect of co-administration of the uricosuric drug probenecid on pralatrexate pharmacokinetics was investigated in a Phase 1 clinical study. Co-administration of increasing doses of probenecid resulted in delayed clearance of pralatrexate and a commensurate increase in exposure. Due to the contribution of renal excretion (approximately 34%) to the overall clearance of pralatrexate, concomitant administration of drugs that are subject to substantial renal clearance (eg, NSAIDs, trimethoprim/sulfamethoxazole) may result in delayed clearance of pralatrexate. |
| References |
|
| Additional Infomation |
Therapeutic Uses
Aminopterin/ analogs & derivatives; Folic Acid Antagonists Pralatrexate is indicated for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma (PTCL). This indication is based on overall response rate. Clinical benefit such as improvement in progression free survival or overall survival has not been demonstrated. /Included in US product label/ T-cell lymphomas (TCL) are characterized by poor response to chemotherapy and generally poor outcome. While molecular profiling has identified distinct biological subsets and therapeutic targets in B-cell lymphomas, the molecular characterization of TCL has been slower. Surface markers expressed on malignant T-cells, such as CD2, CD3, CD4, CD25, and CD52 were the first TCL-specific therapeutic targets to be discovered. However, the presence of these receptors on normal T-cells means that monoclonal antibody (mAb)- or immunotoxin (IT)-based therapy in TCL inevitably results in variable degrees of immunosuppression. Thus, although some mAbs/IT have significant activity in selected subsets of TCL, more specific agents that target signaling pathways preferentially activated in malignant T-cells are needed. One such novel class of agents is represented by the histone deacetylase (HDAC) inhibitors. These molecules selectively induce apoptosis in a variety of transformed cells, including malignant T-cells, both in vitro and in vivo. Several HDAC inhibitors have been studied in TCL with promising results, and have recently been approved for clinical use. Immunomodulatory drugs, such as interferons and Toll Receptor (TLR) agonists have significant clinical activity in TCL, and are particularly important in the treatment of primary cutaneous subtypes (CTCL). Although most classical cytotoxic drugs have limited efficacy against TCL, agents that inhibit purine and pyrimidine metabolism, known as nucleoside analogues, and novel antifolate drugs, such as pralatrexate, are highly active in TCL. With improved molecular profiling of TCL novel pharmacological agents with activity in TCL are now being discovered at an increasingly rapid pace. Clinical trials are in progress and these agents are being integrated in combination therapies for TCL, both in the relapsed/refractory setting as well as front line. Drug Warnings FOLOTYN can suppress bone marrow function, manifested by thrombocytopenia, neutropenia, and anemia. Dose modifications are based on ANC and platelet count prior to each dose. Treatment with FOLOTYN may cause mucositis. If /greater than or equal to/ Grade 2 mucositis is observed, dose should be modified. Patients should be instructed to take folic acid and receive vitamin B12 to potentially reduce treatment-related hematological toxicity and mucositis. ... Patients should take low-dose oral folic acid on a daily basis. Folic acid should be initiated during the 10-day period preceding the first dose of FOLOTYN, and dosing should continue during the full course of therapy and for 30 days after the last dose of FOLOTYN. Patients should also receive a vitamin B12 intramuscular injection no more than 10 weeks prior to the first dose of FOLOTYN and every 8-10 weeks thereafter. Subsequent vitamin B12 injections may be given the same day as treatment with FOLOTYN. Although FOLOTYN has not been formally tested in patients with renal impairment, caution is advised when administering FOLOTYN to patients with moderate to severe impairment. Monitor patients for renal function and systemic toxicity due to increased drug exposure. For more Drug Warnings (Complete) data for Pralatrexate (10 total), please visit the HSDB record page. Pharmacodynamics Pralatrexate is a folate analog that inhibits folate metabolism, thus impeding the synthesis of amino acids and nucleic acid. Additionally, pralatrexate also competes for enzymatic processing by folyopolyglutamate synthase (FPGS)with folate to increase cellular retention. Compared to methotrexate, pralatrexate binds to the reduced folate carrier protein-1 (RFC-1) for cellular uptake with 10-times the affinity and is a more potent substrate for FPGS. The Km value for RFC-1 was calculated to be 0.3 μmol/L and 4.8 μmol/L for pralatrexate and methotrexate respectively, while the Km value for FPGS was estimated to be 5.9 and 32.3 µmol/l for pralatrexate and methotrexate respectively. As a result, pralatrexate is more cytotoxic and better retained in cancer cells. Due to its anti-folate activity, pralatrexate's main toxicity is manifested as mucositis that can require dose interruption or reduction. In 5 patients with non-small-cell lung carcinoma receiving a supratherapeutic dose of 230 mg/m2, the mean change from pre-injection QTcF interval at the end of infusion was 6.1 ms (90%CI: -0.6, 12.7), and at 1-hour post-injection was 7.8 ms (90%CI: 3.0, 12.6). However, no patient exceeded a QTcF of 470 msec and exhibited an absolute increase from baseline in QTcF exceeding 30 msec. As well, the study dose far exceeded the target dose for patients with peripheral T-cell lymphoma and pralatrexate does not inhibit the human ether-a-go-go-related gene (hERG) K+ channel. Therefore, pralatrexate uses are unlikely to cause cardiac repolarization delays.. |
| Molecular Formula |
C23H23N7O5
|
|---|---|
| Molecular Weight |
477.47
|
| Exact Mass |
477.176
|
| CAS # |
146464-95-1
|
| Related CAS # |
(R)-Pralatrexate;1320211-70-8
|
| PubChem CID |
148121
|
| Appearance |
Light yellow to yellow solid powder
|
| Density |
1.5±0.1 g/cm3
|
| Melting Point |
215 °C(dec.)
|
| Index of Refraction |
1.704
|
| LogP |
0.23
|
| Hydrogen Bond Donor Count |
5
|
| Hydrogen Bond Acceptor Count |
11
|
| Rotatable Bond Count |
10
|
| Heavy Atom Count |
35
|
| Complexity |
809
|
| Defined Atom Stereocenter Count |
1
|
| SMILES |
C#CCC(CC1=CN=C2C(=N1)C(=NC(=N2)N)N)C3=CC=C(C=C3)C(=O)N[C@@H](CCC(=O)O)C(=O)O
|
| InChi Key |
OGSBUKJUDHAQEA-WMCAAGNKSA-N
|
| InChi Code |
InChI=1S/C23H23N7O5/c1-2-3-14(10-15-11-26-20-18(27-15)19(24)29-23(25)30-20)12-4-6-13(7-5-12)21(33)28-16(22(34)35)8-9-17(31)32/h1,4-7,11,14,16H,3,8-10H2,(H,28,33)(H,31,32)(H,34,35)(H4,24,25,26,29,30)/t14?,16-/m0/s1
|
| Chemical Name |
N -(4-{1-[(2,4-diaminopteridin-6-yl)methyl]but-3-yn-1-yl}benzoyl)-L-glutamic acid
|
| Synonyms |
PDX; Pralatrexate; 10-Propargyl-10-deazaaminopterin; trade name: Folotyn.
|
| HS Tariff Code |
2934.99.9001
|
| Storage |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| Solubility (In Vitro) |
|
|||
|---|---|---|---|---|
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 2.5 mg/mL (5.24 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution.
For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 25.0 mg/mL clear DMSO stock solution to 400 μL PEG300 and mix evenly; then add 50 μL Tween-80 to the above solution and mix evenly; then add 450 μL normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 2.5 mg/mL (5.24 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 25.0 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. (Please use freshly prepared in vivo formulations for optimal results.) |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.0944 mL | 10.4719 mL | 20.9437 mL | |
| 5 mM | 0.4189 mL | 2.0944 mL | 4.1887 mL | |
| 10 mM | 0.2094 mL | 1.0472 mL | 2.0944 mL |
*Note: Please select an appropriate solvent for the preparation of stock solution based on your experiment needs. For most products, DMSO can be used for preparing stock solutions (e.g. 5 mM, 10 mM, or 20 mM concentration); some products with high aqueous solubility may be dissolved in water directly. Solubility information is available at the above Solubility Data section. Once the stock solution is prepared, aliquot it to routine usage volumes and store at -20°C or -80°C. Avoid repeated freeze and thaw cycles.
Calculation results
Working concentration: mg/mL;
Method for preparing DMSO stock solution: mg drug pre-dissolved in μL DMSO (stock solution concentration mg/mL). Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug.
Method for preparing in vivo formulation::Take μL DMSO stock solution, next add μL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O,mix and clarify.
(1) Please be sure that the solution is clear before the addition of next solvent. Dissolution methods like vortex, ultrasound or warming and heat may be used to aid dissolving.
(2) Be sure to add the solvent(s) in order.
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT02594267 | Completed | Drug: Pralatrexate Injection | Peripheral T-Cell Lymphoma (PTCL) | Acrotech Biopharma Inc. | November 10, 2015 | Phase 1 |
| NCT03355768 | Withdrawn | Drug: Romidepsin Drug: Pralatrexate |
Lymphoma, T-Cell, Peripheral | Jennifer Amengual | September 1, 2018 | Phase 3 |
| NCT03598998 | Active, not recruiting | Biological: Pembrolizumab Drug: Pralatrexate |
Anaplastic Large Cell Lymphoma Nodal Peripheral T-Cell Lymphoma With TFH Phenotype |
City of Hope Medical Center | February 4, 2019 | Phase 1 Phase 2 |
| NCT03240211 | Recruiting | Drug: Pembrolizumab Drug: Pralatrexate |
PTCL CTCL |
University of Virginia | February 2, 2022 | Phase 1 |
 |
|---|
 |
 |