
| Size | Price | Stock | Qty |
|---|---|---|---|
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
Purity: ≥98%
Rosiglitazone (HSDB-7555; BRL-49653; TDZ-01; TDZ01; trade name Avandia) is an approved antidiabetic drug of the thiazolidinedione class with antidiabetic properties and potential antineoplastic activity. It is also a potent insulin sensitizer with IC50s of 12, 4 and 9 nM for rat, 3T3-L1 and human adipocytes, respectively. It is also a selective PPARγ agonist with EC50s of 30 nM, 100 nM and 60 nM for PPARγ1, PPARγ2, and PPARγ, respectively.
| Targets |
PPARγ (Kd = 40 nM); PPARγ (EC50 = 60 nM); TRPC5 (EC50 = 30 μM); TRPM3
|
|---|---|
| ln Vitro |
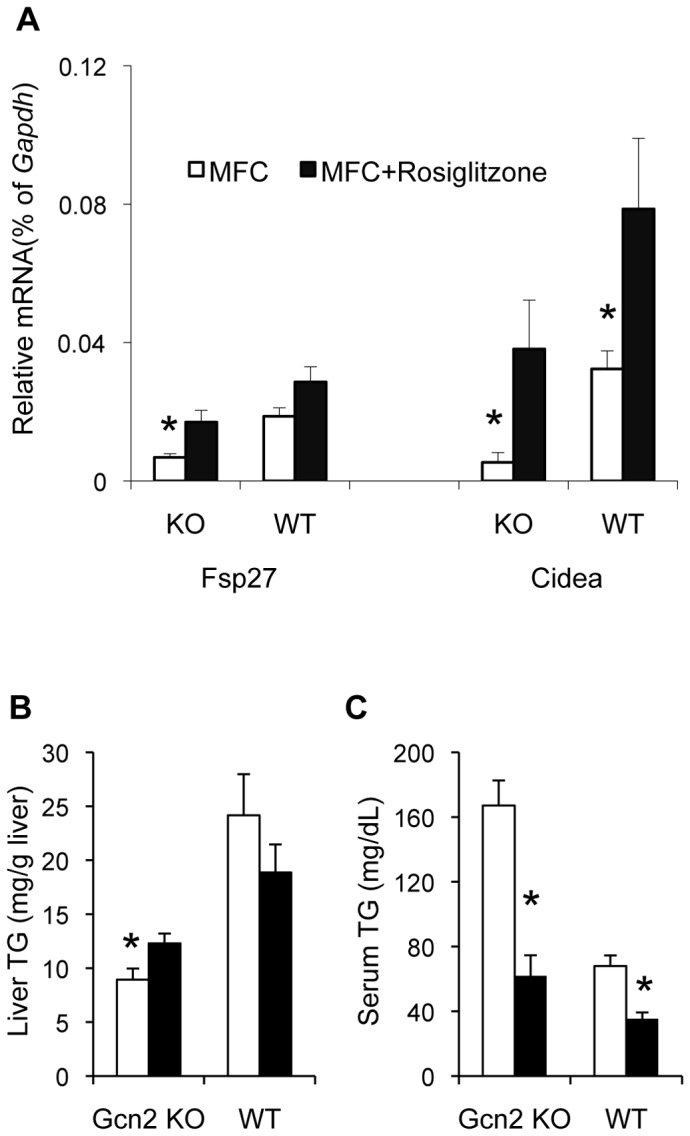
Pluripotent C3H10T1/2 stem cells are differentiated into adipocytes by rosiglitazone (0.1–10 μM, 72 h) [1]. When combined with the NF-α1 promoter, rosiglitazone (1 μM, 24 h) stimulates PPARγ, which in turn activates gene transcription in neurons [3]. Hippocampal neurons and Neuro2A cells are shielded from oxidative stress by rosiglitazone (1 μM, 24 hours), which also increases BCL-2 expression in an NF-κ1-dependent way [3]. With IC50 values of 9.5 and 4.6 μM, rosiglitazone (0.01-100 μM, 15 minutes) inhibits TRPM3, hence preventing PregS- and nifedipine-induced activity, respectively [4]. The proliferation of ovarian cancer cells is inhibited by rosiglitazone (0.5-50 μM, 7 days) [7]. In A2780 and SKOV3 cells, rosiglitazone (5 μM, 7 days) suppresses Olaparib-induced cellular senescence alterations and stimulates apoptosis [7].
|
| ln Vivo |
In diabetic rats, oral rosiglitazone (5 mg/kg, once day for 8 weeks) lowers blood glucose levels [5]. By activating PPARγ and RXRα, rosiglitazone (ip, 3 mg/kg/day) lowers blood glucose and inhibits airway inflammation brought on by M1 macrophage polarization in male Wistar rats [6]. In A2780 and SKOV3 animal subcutaneous xenograft models, rosiglitazone (ip, 10 mg/kg, every 2 days) suppresses the growth of subcutaneous ovarian cancer [7].
|
| Enzyme Assay |
Here, we report that thiazolidinediones are potent and selective activators of peroxisome proliferator-activated receptor gamma (PPAR gamma), a member of the nuclear receptor superfamily recently shown to function in adipogenesis. The most potent of these agents, BRL49653, binds to PPAR gamma with a Kd of approximately 40 nM. Treatment of pluripotent C3H10T1/2 stem cells with BRL49653 results in efficient differentiation to adipocytes. These data are the first demonstration of a high affinity PPAR ligand and provide strong evidence that PPAR gamma is a molecular target for the adipogenic effects of thiazolidinediones. Furthermore, these data raise the intriguing possibility that PPAR gamma is a target for the therapeutic actions of this class of compounds.[1]
cDNA encoding amino acids 174-475 of PPARγ1 is amplified via polymerase chain reaction and inserted into bacterial expression vector pGEX-2T. GST-PPARγ LBD is expressed in BL21(DE3)plysS cells and extracts. For saturation binding analysis, bacterial extracts (100 μg of protein) are incubated at 4°C for 3 h in buffer containing 10 mM Tris (pH 8.0), 50 mM KCl, 10 mM dithiothreitol with [3H]-BRL49653 (specific activity, 40 Ci/mmol) in the presence or absence of unlabeled Rosiglitazone. Bound is separated from free radioactivity by elution through 1-mL Sephadex G-25 desalting columns. Bound radioactivity eluted in the column void volume and is quantitated by liquid scintillation counting[1]. |
| Cell Assay |
Cell Proliferation Assay[7]
Cell Types: A2780 and SKOV3 cells Tested Concentrations: 0.5-50 μM Incubation Duration: 1-7 days Experimental Results: Inhibited cell proliferation in a time‑dependent and concentration‑dependent manner. Western Blot Analysis[3] Cell Types: Hippocampal neurons Tested Concentrations: 1 μM Incubation Duration: 24 h Experimental Results: Increased NF-α1 and BCL-2 protein level. |
| Animal Protocol |
Animal/Disease Models: Streptozotocin (STZ)-induced diabetic rats[5]
Doses: 5 mg/kg Route of Administration: Oral administration, daily for 8 weeks. Experimental Results: diminished IL-6, TNF-α, and VCAM-1 levels in diabetic group. Displayed lower levels of lipid peroxidation and NOx with an increase in aortic GSH and SOD levels compared to diabetic groups. Animal/Disease Models: Male Wistar rats[6] Doses: 3 mg/kg/day Route of Administration: intraperitoneal (ip)injection, twice a day, 6 days Consecutive per week for 12 weeks Experimental Results: Ameliorated emphysema, elevated PEF, and higher level of total cells, neutrophils and cytokines (TNF-α and IL-1β) induced by cigarette smoke (CS). Inhibited CS-induced M1 macrophage polarization and diminished the ratio of M1/M2. |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion
The absolute bioavailability of rosiglitazone is 99%. Peak plasma concentrations are observed about 1 hour after dosing. Administration of rosiglitazone with food resulted in no change in overall exposure (AUC), but there was an approximately 28% decrease in Cmax and a delay in Tmax (1.75 hours). These changes are not likely to be clinically significant; therefore, rosiglitazone may be administered with or without food. Maximum plasma concentration (Cmax) and the area under the curve (AUC) of rosiglitazone increase in a dose-proportional manner over the therapeutic dose range. Following oral or intravenous administration of [14C]rosiglitazone maleate, approximately 64% and 23% of the dose was eliminated in the urine and in the feces, respectively. 17.6 L [oral volume of distribution Vss/F] 13.5 L [population mean, pediatric patients] Oral clearance (CL) = 3.03 ± 0.87 L/hr [1 mg Fasting] Oral CL = 2.89 ± 0.71 L/hr [2 mg Fasting] Oral CL = 2.85 ± 0.69 L/hr [8 mg Fasting] Oral CL = 2.97 ± 0.81 L/hr [8 mg Fed] 3.15 L/hr [Population mean, Pediatric patients] In a study in healthy volunteers, the absorption of rosiglitazone was relatively rapid, with 99% oral bioavailability after oral absorption. Severe forms of non-alcoholic fatty liver disease (NAFLD) adversely affect the liver physiology and hence the pharmacokinetics of drugs. Here, we investigated the effect of NAFLD on the pharmacokinetics of rosiglitazone, an insulin sensitizer used in the treatment of type 2 diabetes. Male C57BL/6 mice were divided into two groups. The first group (n=14) was fed with normal chow feed and the second group (n=14) was fed with 60% high-fat diet (HFD) and 40% high fructose liquid (HFL) for 60 days to induce NAFLD. The development of NAFLD was confirmed by histopathology, liver triglyceride levels and biochemical estimations, and used for pharmacokinetic investigations. Rosiglitazone was administered orally at 30 mg/kg dose. At predetermined time points, blood was collected and rosiglitazone concentrations were determined using LC/MS/MS. Plasma concentrations were subjected to non-compartmental analysis using Phoenix WinNonlin (6.3), and the area under the plasma concentration-time curve (AUC) was calculated by the linear-up log-down method. HFD and HFL diet successfully induced NAFLD in mice. Rosiglitazone pharmacokinetics in NAFLD animals were altered significantly as compared to healthy mice. Rosiglitazone exposure increased significantly in NAFLD mice (2.5-fold higher AUC than healthy mice). The rosiglitazone oral clearance was significantly lower and the mean plasma half-life was significantly longer in NAFLD mice as compared to healthy mice. The NAFLD mouse model showed profound effects on rosiglitazone pharmacokinetics. The magnitude of change in rosiglitazone pharmacokinetics is similar to that observed in humans with moderate to severe liver disease. The present animal model can be utilized to study the NAFLD-induced changes in the pharmacokinetics of different drugs. The absolute bioavailability of rosiglitazone is 99%. Peak plasma concentrations are observed about 1 hour after dosing. Administration of rosiglitazone with food resulted in no change in overall exposure (AUC), but there was an approximately 28% decrease in Cmax and a delay in Tmax (1.75 hours). These changes are not likely to be clinically significant; therefore, Avandia may be administered with or without food. The mean (CV%) oral volume of distribution (Vss/F) of rosiglitazone is approximately 17.6 (30%) liters, based on a population pharmacokinetic analysis. Rosiglitazone is approximately 99.8% bound to plasma proteins, primarily albumin. For more Absorption, Distribution and Excretion (Complete) data for Rosiglitazone (8 total), please visit the HSDB record page. Metabolism / Metabolites Hepatic. Rosiglitazone is extensively metabolized in the liver to inactive metabolites via N-demethylation, hydroxylation, and conjugation with sulfate and glucuronic acid. In vitro data have shown that Cytochrome (CYP) P450 isoenzyme 2C8 (CYP2C8) and to a minor extent CYP2C9 are involved in the hepatic metabolism of rosiglitazone. The main metabolites observed in humans are also observed in rats; however, the clearance in rats was almost ten times higher than in humans, probably due to the higher levels of CYP2C in rat microsomes. In vitro data demonstrate that rosiglitazone is predominantly metabolized by Cytochrome P450 (CYP) isoenzyme 2C8, with CYP2C9 contributing as a minor pathway. Rosiglitazone is extensively metabolized with no unchanged drug excreted in the urine. The major routes of metabolism were N-demethylation and hydroxylation, followed by conjugation with sulfate and glucuronic acid. All the circulating metabolites are considerably less potent than parent and, therefore, are not expected to contribute to the insulin-sensitizing activity of rosiglitazone. Rosiglitazone has known human metabolites that include N-Desmethylrosiglitazone, ortho-hydroxyrosiglitazone, and para-hydroxyrosiglitazone. Biological Half-Life 3-4 hours (single oral dose, independent of dose) The elimination half-life of rosiglitazone was 3-4 hours and was independent of dose. The time to Cmax and the elimination half-life for two metabolites in plasma were significantly longer than for rosiglitazone itself (4-6 hours versus 0.5-1 hours, and about 5 days versus 3-7 hours). The plasma half life of (14)C-related material ranged from 103 to 158 hours. |
| Toxicity/Toxicokinetics |
Toxicity Summary
IDENTIFICATION AND USE: Rosiglitazone is a solid. It is used as an antidiabetic agent as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus. HUMAN STUDIES: Thiazolidinediones, including rosiglitazone, alone or in combination with other antidiabetic agents, can cause fluid retention and may lead to or exacerbate congestive heart failure (CHF). Use of thiazolidinediones is associated with an approximately twofold increased risk of CHF. No evidence of hepatotoxicity has been noted with rosiglitazone in clinical studies to date, including a long-term (4-6 years) study in patients with recently diagnosed type 2 diabetes mellitus. However, hepatitis, elevations in hepatic enzymes to at least 3 times the upper limit of normal, and liver failure with or without fatalities have been reported during postmarketing experience with rosiglitazone. Rosiglitazone was not mutagenic or clastogenic in the in vitro chromosome aberration test in human lymphocytes. ANIMAL STUDIES: Rosiglitazone was not carcinogenic in the mouse. There was an increase in incidence of adipose hyperplasia in the mouse at doses >/= 1.5 mg/kg/day. Heart weights were increased in mice (3 mg/kg/day), rats (5 mg/kg/day), and dogs (2 mg/kg/day) with rosiglitazone treatments. Effects in juvenile rats were consistent with those seen in adults. Morphometric measurement indicated that there was hypertrophy in cardiac ventricular tissues, which may be due to increased heart work as a result of plasma volume expansion. Rosiglitazone had no effects on mating or fertility of male rats given up to 40 mg/kg/day. In juvenile rats dosed from 27 days of age through to sexual maturity (at up to 40 mg/kg/day), there was no effect on male reproductive performance, or on estrous cyclicity, mating performance, or pregnancy incidence in females. Rosiglitazone was not mutagenic or clastogenic in the in vitro bacterial assays for gene mutation, the in vivo mouse micronucleus test, and the in vivo/in vitro rat UDS assay. There was a small (about 2-fold) increase in mutation in the in vitro mouse lymphoma assay in the presence of metabolic activation. Hepatotoxicity In contrast to troglitazone, rosiglitazone is not associated with an increased frequency of aminotransferase elevations during therapy. In clinical trials, ALT elevations above 3 times the ULN occurred in only 0.25% of patients on rosiglitazone, compared to 0.25% of placebo recipients (and 1.9% of troglitazone recipients in similar studies). In addition, clinically apparent liver injury attributed to rosiglitazone is very rare, fewer than a dozen cases having been described in the literature despite extensive use of this agent. The liver injury usually arises between 1 and 12 weeks after starting therapy (thus, a shorter latency than typically occurs with troglitazone) and all patterns of serum enzyme elevations have been described including hepatocellular, cholestatic and mixed. Allergic phenomena are rare and autoantibodies have not been typically present. Fatal instances have been reported usually in cases with a hepatocellular pattern of injury. In most instances, recovery is complete within 1 to 2 months. Likelihood score: C (probable rare cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of rosiglitazone during breastfeeding. Rosiglitazone is over 99% protein bound in plasma, so it is unlikely to pass into breastmilk in clinically important amounts. The manufacturer recommends avoiding breastfeeding during rosiglitazone use, so pioglitazone might be a better choice of the drugs in this class for nursing mothers. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 99.8% bound to plasma proteins, primarily albumin. Interactions An inhibitor of CYP2C8 (e.g., gemfibrozil) may increase the AUC of rosiglitazone and an inducer of CYP2C8 (e.g., rifampin) may decrease the AUC of rosiglitazone. Therefore, if an inhibitor or an inducer of CYP2C8 is started or stopped during treatment with rosiglitazone, changes in diabetes treatment may be needed based upon clinical response. /The authors/ investigated the possible effect of ketoconazole on the pharmacokinetics of rosiglitazone in humans. Ten healthy Korean male volunteers were treated twice daily for 5 days with 200 mg ketoconazole or with placebo, using a randomized, open-label, two-way crossover study. On day 5, a single dose of 8 mg rosiglitazone was administered orally, and plasma rosiglitazone concentrations were measured. Ketoconazole increased the mean area under the plasma concentration-time curve for rosiglitazone by 47%[P = 0.0003; 95% confidence interval (CI) 23, 70] and the mean elimination half-life from 3.55 to 5.50 hr (P = 0.0003; 95% CI in difference 1.1, 2.4). The peak plasma concentration of rosiglitazone was increased by ketoconazole treatment by 17% (P = 0.03; 95% CI 5, 29). The apparent oral clearance of rosiglitazone decreased by 28% after ketoconazole treatment (P = 0.0005; 95% CI 18, 38). This study revealed that ketoconazole affected the disposition of rosiglitazone in humans, probably by the inhibition of CYP2C8 and CYP2C9, leading to increasing rosiglitazone concentrations that could increase the efficacy of rosiglitazone or its adverse events. Endothelial dysfunction is implicated in the initiation and progression of atherosclerosis. Whether atorvastatin combined with rosiglitazone has synergistic effects on endothelial function improvement in the setting of dyslipidemia is unknown. Dyslipidemia rat model was produced with high-fat and high-cholesterol diet administration. Thereafter, atorvastatin, rosiglitazone or atorvastatin combined with rosiglitazone were prescribed for 2 weeks. At baseline, 6 weeks of dyslipidemia model production, and 2 weeks of medical intervention, fasting blood was drawn for parameters of interest evaluation. At the end, myocardium was used for 15-deoxy-delta-12,14-PGJ2 (15-d-PGJ2) assessment. Initially, there was no significant difference of parameters between sham and dyslipidemia groups. With 6 weeks' high-fat and high-cholesterol diet administration, as compared to sham group, serum levels of triglyceride (TG), total cholesterol (TC) and low density lipoprotein-cholesterol (LDL-C) were significantly increased. Additionally, nitric oxide (NO) production was reduced and serum levels of malondialdehyde (MDA), C-reactive protein (CRP) and asymmetric dimethylarginine (ADMA) were profoundly elevated in dyslipidemia group. After 2 weeks' medical intervention, lipid profile was slightly improved in atorvastatin and combined groups as compared to control group. Nevertheless, in comparison to control group, NO production was profoundly increased and serum levels of MDA, CRP and ADMA were significantly decreased with atorvastatin or rosiglitazone therapy. 15-d-PGJ2 expression of myocardium was also significantly elevated with atorvastatin or rosiglitazone treatment. Notably, these effects were further enhanced with combined therapy, suggesting that atorvastatin and rosiglitazone had synergistic effects on endothelial protection, and inflammation and oxidation amelioration. Atorvastatin and rosiglitazone therapy had synergistic effects on endothelium protection as well as amelioration of oxidative stress and inflammatory reaction in rats with dyslipidemia. Avandia (2 mg twice daily) taken concomitantly with glyburide (3.75 to 10 mg/day) for 7 days did not alter the mean steady-state 24-hour plasma glucose concentrations in diabetic patients stabilized on glyburide therapy. Repeat doses of Avandia (8 mg once daily) for 8 days in healthy adult Caucasian subjects caused a decrease in glyburide AUC and Cmax of approximately 30%. In Japanese subjects, glyburide AUC and Cmax slightly increased following coadministration of Avandia. Rifampin administration (600 mg once a day), an inducer of CYP2C8, for 6 days is reported to decrease rosiglitazone AUC by 66%, compared with the administration of rosiglitazone (8 mg) alone. |
| References |
|
| Additional Infomation |
Therapeutic Uses
Antidiabetic agent /CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Rosiglitazone is included in the database. Rosiglitazone is used as monotherapy or in combination with a sulfonylurea, metformin hydrochloride, or a sulfonylurea and metformin as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus. Rosiglitazone in fixed combination with metformin hydrochloride is used as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus. Rosiglitazone also is used in fixed combination with glimepiride as an adjunct to diet and exercise for the management of type 2 diabetes mellitus. /Included in US product label/ /EXPL THER/ 1-Methyl-4-phenylpyridinium ion (MPP(+)), an inhibitor of mitochondrial complex I, has been widely used as a neurotoxin because it elicits a severe Parkinson's disease-like syndrome with elevation of intracellular reactive oxygen species (ROS) level and apoptotic death. Rosiglitazone, a peroxisome proliferator-activated receptor (PPAR)-gamma agonist, has been known to show various non-hypoglycemic effects, including anti-inflammatory, anti-atherogenic, and anti-apoptotic. In the present study, /the authors/ investigated the protective effects of rosiglitazone on MPP(+) induced cytotoxicity in human neuroblastoma SH-SY5Y cells, as well as underlying mechanism. /Their/ results suggested that the protective effects of rosiglitazone on MPP(+) induced apoptosis may be ascribed to its anti-oxidative properties, anti-apoptotic activity via inducing expression of SOD and catalase and regulating the expression of Bcl-2 and Bax. These data indicated that rosiglitazone might provide a valuable therapeutic strategy for the treatment of progressive neurodegenerative disease such as Parkinson's disease. Drug Warnings /BOXED WARNING/ WARNING: CONGESTIVE HEART FAILURE. Thiazolidinediones, including rosiglitazone, cause or exacerbate congestive heart failure in some patients. After initiation of Avandia, and after dose increases, observe patients carefully for signs and symptoms of heart failure (including excessive, rapid weight gain; dyspnea; and/or edema). If these signs and symptoms develop, the heart failure should be managed according to current standards of care. Furthermore, discontinuation or dose reduction of Avandia must be considered. Avandia is not recommended in patients with symptomatic heart failure. Initiation of Avandia in patients with established NYHA Class III or IV heart failure is contraindicated. Thiazolidinediones, including rosiglitazone, alone or in combination with other antidiabetic agents, can cause fluid retention and may lead to or exacerbate congestive heart failure (CHF). Use of thiazolidinediones is associated with an approximately twofold increased risk of CHF. Patients should be observed for signs and symptoms of CHF (e.g., dyspnea, rapid weight gain, edema, unexplained cough or fatigue), especially during initiation of therapy and dosage titration. If signs and symptoms of CHF develop, the disorder should be managed according to current standards of care. In addition, a decrease in the dosage of rosiglitazone or discontinuance of the drug should be considered. Thiazolidinedione use is associated with bone loss and fractures in women and possibly in men with type 2 diabetes mellitus. In long-term comparative clinical trials in patients with type 2 diabetes mellitus, the incidence of bone fracture was increased in patients (particularly women) receiving rosiglitazone versus comparator agents (glyburide and/or metformin). Such effects were noted after the first year of treatment and persisted throughout the study. The majority of fractures observed in patients taking thiazolidinediones were in a distal upper limb (i.e., forearm, hand, wrist) or distal lower limb (i.e., foot, ankle, fibula, tibia). In an observational study in the United Kingdom in men and women (mean age: 60.7 years) with diabetes mellitus, use of pioglitazone or rosiglitazone for approximately 12-18 months (as estimated from prescription records) was associated with a twofold to threefold increase in fractures, particularly of the hip and wrist. The overall risk of fracture was similar among men and women and was independent of body mass index, comorbid conditions, diabetic complications, duration of diabetes mellitus, and use of other oral antidiabetic drugs.145 Risk of fractures should be considered when initiating or continuing thiazolidinedione therapy in female patients with type 2 diabetes mellitus. Bone health should be assessed and maintained according to current standards of care. Although increased risk of fracture may also apply to men, the risk appears to be higher among women than men. Because rosiglitazone requires endogenous insulin for activity, it should not be used in patients with type 1 diabetes mellitus or diabetic ketoacidosis. For more Drug Warnings (Complete) data for Rosiglitazone (19 total), please visit the HSDB record page. Pharmacodynamics When rosiglitazone is used as monotherapy, it is associated with increases in total cholesterol, LDL, and HDL. It is also associated with decreases in free fatty acids. Increases in LDL occurred primarily during the first 1 to 2 months of therapy with AVANDIA and LDL levels remained elevated above baseline throughout the trials. In contrast, HDL continued to rise over time. As a result, the LDL/HDL ratio peaked after 2 months of therapy and then appeared to decrease over time. |
| Molecular Formula |
C18H19N3O3S
|
|---|---|
| Molecular Weight |
357.43
|
| Exact Mass |
357.114
|
| Elemental Analysis |
C, 60.49; H, 5.36; N, 11.76; O, 13.43; S, 8.97
|
| CAS # |
122320-73-4
|
| Related CAS # |
Rosiglitazone maleate;155141-29-0;Rosiglitazone hydrochloride;302543-62-0;Rosiglitazone potassium;316371-84-3;Rosiglitazone-d3;1132641-22-5
|
| PubChem CID |
77999
|
| Appearance |
Colorless crystals from methanol
|
| Density |
1.3±0.1 g/cm3
|
| Boiling Point |
585.0±35.0 °C at 760 mmHg
|
| Melting Point |
153-155ºC
|
| Flash Point |
307.6±25.9 °C
|
| Vapour Pressure |
0.0±1.6 mmHg at 25°C
|
| Index of Refraction |
1.642
|
| LogP |
2.56
|
| Hydrogen Bond Donor Count |
1
|
| Hydrogen Bond Acceptor Count |
6
|
| Rotatable Bond Count |
7
|
| Heavy Atom Count |
25
|
| Complexity |
469
|
| Defined Atom Stereocenter Count |
0
|
| SMILES |
S1C(N([H])C(C1([H])C([H])([H])C1C([H])=C([H])C(=C([H])C=1[H])OC([H])([H])C([H])([H])N(C([H])([H])[H])C1=C([H])C([H])=C([H])C([H])=N1)=O)=O
|
| InChi Key |
YASAKCUCGLMORW-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C18H19N3O3S/c1-21(16-4-2-3-9-19-16)10-11-24-14-7-5-13(6-8-14)12-15-17(22)20-18(23)25-15/h2-9,15H,10-12H2,1H3,(H,20,22,23)
|
| Chemical Name |
5-(4-(2-(methyl(pyridin-2-yl)amino)ethoxy)benzyl)thiazolidine-2,4-dione
|
| Synonyms |
HSDB7555; TDZ 01; HSDB 7555; HSDB-7555; BRL 49653; BRL49653; BRL-49653; TDZ-01; TDZ01; Rosiglitazone. trade name Avandia; rosiglitazone; 122320-73-4; Avandia; Rosiglizole; 5-(4-(2-(Methyl(pyridin-2-yl)amino)ethoxy)benzyl)thiazolidine-2,4-dione; Brl-49653; Brl 49653; Rezult; .
|
| HS Tariff Code |
2934.99.9001
|
| Storage |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| Solubility (In Vitro) |
|
|||
|---|---|---|---|---|
| Solubility (In Vivo) |
Solubility in Formulation 1: 2.5 mg/mL (6.99 mM) in 10% DMSO + 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), suspension solution; with sonication.
For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 25.0 mg/mL clear DMSO stock solution to 900 μL of corn oil and mix evenly. Solubility in Formulation 2: ≥ 2.5 mg/mL (6.99 mM) (saturation unknown) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. View More
Solubility in Formulation 3: ≥ 2.5 mg/mL (6.99 mM) (saturation unknown) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. Solubility in Formulation 4: ≥ 2.08 mg/mL (5.82 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 20.8 mg/mL clear DMSO stock solution to 400 μL of PEG300 and mix evenly; then add 50 μL of Tween-80 to the above solution and mix evenly; then add 450 μL of normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 5: ≥ 2.08 mg/mL (5.82 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 20.8 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 6: 4% DMSO+30% PEG 300+5% Tween 80+ddH2O: 5mg/mL Solubility in Formulation 7: 10 mg/mL (27.98 mM) in 0.5% CMC-Na/saline water (add these co-solvents sequentially from left to right, and one by one), suspension solution; with ultrasonication. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.7978 mL | 13.9888 mL | 27.9775 mL | |
| 5 mM | 0.5596 mL | 2.7978 mL | 5.5955 mL | |
| 10 mM | 0.2798 mL | 1.3989 mL | 2.7978 mL |
*Note: Please select an appropriate solvent for the preparation of stock solution based on your experiment needs. For most products, DMSO can be used for preparing stock solutions (e.g. 5 mM, 10 mM, or 20 mM concentration); some products with high aqueous solubility may be dissolved in water directly. Solubility information is available at the above Solubility Data section. Once the stock solution is prepared, aliquot it to routine usage volumes and store at -20°C or -80°C. Avoid repeated freeze and thaw cycles.
Calculation results
Working concentration: mg/mL;
Method for preparing DMSO stock solution: mg drug pre-dissolved in μL DMSO (stock solution concentration mg/mL). Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug.
Method for preparing in vivo formulation::Take μL DMSO stock solution, next add μL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O,mix and clarify.
(1) Please be sure that the solution is clear before the addition of next solvent. Dissolution methods like vortex, ultrasound or warming and heat may be used to aid dissolving.
(2) Be sure to add the solvent(s) in order.
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT01100619 | Completed | Drug: rosiglitazone Drug: XL184 |
Papillary Thyroid Cancer Follicular Thyroid Cancer |
Exelixis | April 2010 | Phase 1 |
| NCT01706211 | Completed | Drug: BRL 49653C Drug: Placebo |
Diabetes Mellitus Non Insulin Dependent Oral Agent Therapy |
National Taiwan University Hospital | October 1998 | Phase 3 |
| NCT02694874 | Completed | Drug: Rosiglitazone Drug: Placebo |
Malaria | Centro de Investigacao em Saude de Manhica |
February 2016 | Not Applicable |
| NCT00785213 | Completed Has Results | Drug: Rosiglitazone 4 mg Tablets Drug: Quinine Sulfate 324 mg Capsules |
Healthy | Mutual Pharmaceutical Company, Inc. | September 2008 | Phase 1 |
 |
|---|
|
|
|
|---|
|
|