
| Size | Price | Stock | Qty |
|---|---|---|---|
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
Purity: ≥98%
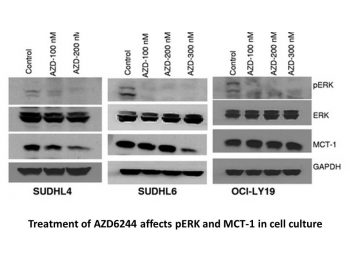
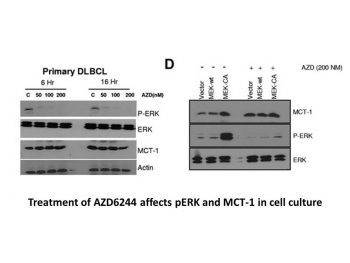
Selumetinib (also known as AZD6244; ARRY-142886; Koselugo) is a novel, potent, highly selective and orally bioavailable small molecule MEK1 inhibitor with anticancer activity. It is an approved drug for the treatment of children with neurofibromatosis type I, a genetic nervous system disorder that causes tumors to develop on nerves. In cell-free assays, selumetinib inhibits MEK1 with an IC50 of 14 nM and ERK1/2 phosphorylation with an IC50 of 10 nM, but it has no inhibitory effect on p38, MKK6, EGFR, ErbB2, ERK2, B-Raf, etc. It has strong in vivo antitumor efficacy and excellent in vitro anti-proliferative activity.
| Targets |
MEK2; MEK1 (IC50 = 14 nM); MEK (IC50 = 12 nM)
|
|---|---|
| ln Vitro |
Selumetinib is not ATP-competitive and inhibits ERK1/2 phosphorylation at IC50 levels under 40 nM. Through the inhibition of ERK1/2 and p90RSK phosphorylation, as well as the elevation of caspase-3 and caspase-7 cleavage and cleaved poly(ADP)ribose polymerase, AZD6244 also slows the growth of primary HCC cells. The p38, c-Jun-NH2-kinase, phosphatidylinositol 3-kinase, and MEK5/ERK5 pathways are not significantly impacted by AZD6244. [1] Raf mutations in breast cancer cell lines and Ras mutations in NSCLC cell lines are both responsive to AZD6244.[2]
|
| ln Vivo |
Selumetinib significantly inhibits phosphorylation of ERK1/2 in 2-1318, 5-1318, 26-1004 and 4-1318 xenografts and induces apoptosis in primary 2-1318 cells by activating the caspase pathway. At a dose of 100 mg/kg, AZD6244 could slow the growth of the tumor in the HT-29 xenograft, a colorectal tumor model with a B-Raf mutation; this tumor growth inhibition is superior to that of Gemcitabine. Apoptosis and the down-regulation of cell cycle regulators like cyclin D1, Cdc-2, CDK2 and 4, cyclin B1, and c-Myc are associated with increased apoptosis, which is why AZD6244 could inhibit the growth of HCC xenograft tumors in the absence of these factors.
|
| Enzyme Assay |
MEK1. [3]
NH2-terminal hexahistidine tagged, constitutively active MEK1 (S218D, S222D ΔR4F; ref. 18) was expressed in baculovirus-infected Hi5 insect cells and purified by immobilized metal affinity chromatography, ion exchange, and gel filtration. The activity of MEK1 was assessed by measuring the incorporation of [γ-33P]phosphate from [γ-33P]ATP onto ERK2. The assay was carried out in a 96-well polypropylene plate with an incubation mixture (100 μL) composed of 25 mmol/L HEPES (pH 7.4), 10 mmol/L MgCl2, 5 mmol/L β-glycerolphosphate, 100 μmol/L sodium orthovanadate, 5 mmol/L DTT, 5 nmol/L MEK1, 1 μmol/L ERK2, and 0 to 80 nmol/L compound (final concentration of 1% DMSO). The reactions were initiated by the addition of 10 μmol/L ATP (with 0.5 μC k[γ-33P]ATP/well) and incubated at room temperature for 45 min. An equal volume of 25% trichloracetic acid was added to stop the reaction and precipitate the proteins. Precipitated proteins were trapped onto glass fiber B filter plates, excess labeled ATP was washed off with 0.5% phosphoric acid, and radioactivity was counted in a liquid scintillation counter. ATP dependence was determined by varying the amount of ATP in the reaction mixture. The data were globally fitted using SigmaPlot. Values were calculated using the following equation for noncompetitive inhibition: v = [Vmax × S / (1 + I / Ki)] / (Km + S).[3] ERK2. [3] To measure inhibition of ERK2, the kinase activity of ERK2 was first activated by MEK1. Wild-type (WT) ERK2 containing an NH2-terminal hexahistidine tag was overexpressed in Escherichia coli and purified by immobilized metal affinity chromatography, ion exchange, and gel filtration. To activate WT ERK2, 2 mg WT ERK2 was mixed with 17 μg of constitutively active MEK1 in 4 mL of 25 mmol/L HEPES (pH 7.5) containing 1 mmol/L ATP. The reaction mixture was incubated at room temperature for 40 min, and the addition of two phosphates was confirmed by mass spectrometry. Activated WT ERK2 was further purified by ion exchange. ERK2 activity was assayed as described for constitutively active MEK, using 10 nmol/L activated ERK2. The substrate used was myelin basic protein at a concentration of 1 μmol/L.[3] MEK1 molecules are immunoprecipitated using an anti-MEK1 antibody. When recombinant ERK1 is activated by immuno-isolated MEK1 in a coupled assay with MBP as the end point, MEK kinase activity is calculated. Before being exposed to X-ray film, phosphorylated MBP is resolved on a 14% SDS-PAGE gel and vacuum-dried. |
| Cell Assay |
Cell Viability and Cell Proliferation[1]
Primary HCC cells were plated at a density of 2.0 × 104 per well in growth medium. After 48 h in growth medium, the cell monolayer was rinsed twice with MEM. Cells were treated with various concentrations of AZD6244 (0, 0.5, 1.0, 2.0, 3.0, and 4.0 μmol/L) for 24 or 48 h. Cell viability was determined by the 3-(4,5-dimethylthiazol-2y1)-2,5-diphenyltetrazolium bromide (MTT) assay (32). Cell proliferation was assayed using a bromodeoxyuridine kit (Roche) as described by the manufacturer. Experiments were repeated at least thrice, and the data were expressed as mean ± SE.[1] Detection of Apoptosis[1] Primary HCC cells were grown in eight-chamber slides and treated with 0, 0.5, 1.0, 2.0, 3.0, and 4.0 μmol/L of AZD6244 in SRF medium for 24 h. Cells were fixed with PBS containing 4% formalin solution for 1 h at room temperature and washed with PBS. Apoptosis was detected by the terminal deoxynucleotidyl transferase–mediated dUTP nick-end labeling (TUNEL) assay using the In situ Cell Death Detection kit (Roche) as described by the manufacturer. Apoptotic cells were then visualized under a fluorescent microscope equipped with a FITC filter. The labeling index was obtained by counting the number of positive cells among 500 cells per region. They were expressed as percentage values.[1] At a density of2.0 × 104, cells are seeded. The cells undergo two culture media rinses after 48 hours of incubation. AZD6244 is used to treat cells for 24 or 48 hours at various concentrations. The MTT assay uses 3-(4,5-dimethylthiazol-2y1)-2,5-diphenyltetrazolium bromide to measure the viability of cells. With the help of a bromodeoxyuridine kit, cell proliferation is measured. |
| Animal Protocol |
HCC xenografts in mice homozygous for the SCID (severe combined immunodeficiency) mutation
50 or 100mg/kg Administered via p.o. o investigate the effects of AZD6244 on HCC xenografts, AZD6244 was suspended in water at an appropriate concentration. Mice bearing HCC xenografts were p.o. given, twice a day, with either 100 μL of water (n = 12) or 50 mg (n = 12) or 100 mg (n = 12) of AZD6244 per kilogram of body weight for 21 days, starting from day 7 after tumor implantation. Growth of established tumor xenografts was monitored at least twice weekly by Vernier caliper measurement of the length (a) and width (b) of the tumor. Tumor volume was calculated as (a × b2)/2. Animals were sacrificed 3 h after the last dose of ADZ6244, and body and tumor weights were recorded, with the tumors harvested for analysis.[1] To study the effects of AZD6244 on caspase-3 activation and MEK1/2 phosphorylation, mice bearing HCC tumors (∼800 mm3) were treated with vehicle (n = 4) or 50 mg of AZD6244 per kilogram of body weight (n = 4) for 3 days as described above. Animals were sacrificed 3 h after the last dose, and tumors were harvested and frozen in liquid nitrogen for later analysis. Part of the tumor harvest was fixed in neutral buffer containing 10% formalin for immunohistochemistry.[1] HT-29 human colon carcinoma or BxPC3 human pancreatic tumor fragments were implanted s.c. in the flank of nude mice and allowed to grow to 100 to 150 mg. Mice (n = 10 per group) were randomized to treatment groups to receive vehicle (10 mL/kg and 10% ethanol/10% cremophor EL/80% D5W) or AZD6244/ARRY-142886 (10, 25, 50, or 100 mg/kg, oral, BID) on days 1 to 21. Tumors [(W2 × L) / L] were measured twice weekly. [3] |
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion
Based on several studies investigating selumetinib at various doses in both pediatric and adult populations, the Tmax generally ranges between 1- 1.5 hours. In healthy adults, the mean absolute oral bioavailability was reported to be 62%. Selumetinib should be administered on an empty stomach since food significantly decreases serum concentrations of the drug. Approximately 59% of selumetinib is eliminated in the feces, while 33% is eliminated in the urine. The mean apparent volume of distribution of selumetinib at steady state in pediatric patients ranged from 78 L to 171 L. A study in healthy adult males found a mean apparent volume of distribution of 146 L. Another study observing the pharmacokinetic effects of various selumetinib doses and regimens in select Japanese patients found that the apparent volume of distribution values at steady-state ranged from 73.2 - 148.1 L. The clearance of selumetinib in pediatric patients is 8.8 L/hr. A study in healthy adult males found a clearance value of 15.7 L/hr. Another study observing the pharmacokinetic effects of various selumetinib doses and regimens in select Japanese patients found clearance values that ranged from 9.2 - 15.9 L/hr. Metabolism / Metabolites Selumetinib is heavily metabolized in the liver and the proposed metabolic pathway is as follows: Hydrolysis of selumetinib’s amide functional group produces M15 (AZ13326637), which contains a carboxylic acid. Elimination of the ethanediol moiety from the parent compound results in the formation of the primary amide M14 (AZ12791138) metabolite. Amide hydrolysis transforms M14 into M15, glucuronidation and further oxidation of M14 leads to M2, M6 and M1, and N-demethylation of M14 produces M12. The amide glucuronide (M2) is thought to be the major circulating metabolite. Demethylation of selumetinib produces the pharmacologically active M8 (AZ12442942), and further oxidation of M8 leads to M11. Glucuronidation of M8 produces M3 or M5, and elimination of the ethanediol moiety from M8 results in a primary amide, producing M12. Although the N-demethylated metabolite (M8) accounts for <10% of the circulating metabolites, it is responsible for approximately 21-35% of any observed pharmacological activity. Ribose conjugation transforms M12 into M9, while oxidation of M12 leads to M10 and M13 metabolites. Glucuronidation of M10 produces M1. Direct glucuronidation of selumetinib produces M4 or M7, which can both eventually transform into M3 and M5 metabolites. Biological Half-Life Selumetinib is characterized by a short half-life. The elimination half-life associated with a dose of 25 mg/m2 in pediatric patients is 6.2 hours. In a study observing the pharmacokinetic effects of various selumetinib regimens in select Japanese patients, the half-life ranged from 9.2- 10.6 hours. In other studies where selumetinib 75 mg is administered twice daily, the half-life is reported to be approximately 13 hours. |
| Toxicity/Toxicokinetics |
Hepatotoxicity
In the prelicensure clinical trials conducted in children and adults with neurofibromatosis, serum aminotransferase elevations occurred in 35% of treated subject but rose to above 5 times the upper limit of normal (ULN) in only 4%. However, there were no liver related serious adverse events and no patient had a concurrent elevation in serum aminotransferase and bilirubin levels. The ALT elevations were typically mild and transient and usually resolved even without dose adjustment. There were no instances of clinically apparent liver injury attributed to selumetinib. Since approval and more wide scale availability of selumetinib, there have been no published reports of clinically apparent drug induced liver injury associated with its use in neurofibromatosis, although clinical experience with the drug, particularly with long term therapy, has been limited. However, in studies of experimental therapy with somewhat higher doses of selumetinib in patients with advanced, refractory cancers, liver test abnormalities were common and sometimes graded as severe (ALT above 20 times ULN) and requiring drug discontinuation. Thus, in patients with neurofibromatosis and use of recommended doses of selumetinib, clinically apparent liver injury is rare if it occurs at all. At higher doses, however, selumetinib has been associated with a very high rate of serum enzyme elevations, many of which were in the range suggestive of severe injury. Likelihood score: E* (suspected but unproven rare cause of clinically apparent liver injury). Protein Binding Separate studies investigating selumetinib protein binding found that 96% of selumetinib was bound to serum albumin, while <35% was bound to ɑ-1 acid glycoprotein. Overall, approximately 98.4% of selumetinib is plasma protein bound. |
| References |
[1]. Mol Cancer Ther . 2007 Jan;6(1):138-46. [2]. Mol Cancer Ther . 2010 Jul;9(7):1985-94. [3]. Clin Cancer Res . 2007 Mar 1;13(5):1576-83. [4]. Mol Cancer Ther . 2007 Sep;6(9):2468-76. [5]. Mol Cancer Ther . 2007 Aug;6(8):2209-19. [6]. Clin Cancer Res . 2012 Feb 15;18(4):1051-62. [7]. Int J Oncol . 2012 Aug;41(2):712-20. [8]. J Clin Endocrinol Metab . 2008 Jun;93(6):2194-201. [9]. Proc Natl Acad Sci U S A . 2009 Dec 1;106(48):20411-6. [10]. Cancer Res . 2008 Aug 1;68(15):6145-53. [11]. J Hepatol . 2010 Jan;52(1):79-87. |
| Additional Infomation |
Selumetinib is a member of the class of benzimidazoles that is 1-methyl-1H-benzimidazole which is substituted at positions 4, 5, and 6 by fluorine, (4-bromo-2-chlorophenyl)amino, and N-(2-hydroxyethoxy)aminocarbonyl groups, respectively. It is a MEK1 and MEK2 inhibitor. It has a role as an EC 2.7.11.24 (mitogen-activated protein kinase) inhibitor, an antineoplastic agent and an anticoronaviral agent. It is a member of benzimidazoles, a hydroxamic acid ester, a member of monochlorobenzenes, a member of bromobenzenes, an organofluorine compound and a secondary amino compound.
Activation of the Raf-MEK-ERK signalling pathway is known to be implemented in several types of malignancies; thus, mitogen-activated protein kinase kinase (MEK) inhibitors such as selumetinib are important tools that can target the problematic overactivity of this pathway. Results from clinical trials investigating earlier developed MEK inhibitors were underwhelming. However, selumetinib demonstrated impressive efficacy and tolerability in Phase I trials, leading to its continued investigation for the treatment of various types of tumours in Phase II trials. Currently, the novel MEK 1 / 2 inhibitor, selumetinib, is approved solely for the treatment of Neurofibromatosis type 1 (NF-1) in a limited age group. NF-1 is considered rare, with an estimated incidence of 1/3000 individuals. It is a genetic, autosomal dominant condition resulting from mutations of the NF1 gene, which can lead to various complications, including the development of multiple tumours in the nervous system. Some patients with this disorder develop plexiform neurofibromas (PN); however, this is considered relatively uncommon compared to other variants of NF-1. Luckily, the use of selumetinib in patients with NF-1 have shown efficacy in shrinking associated tumours and is linked to other positive clinical outcomes. Selumetinib was approved by the FDA on April 10, 2020. It was later approved by Health Canada on August 23, 2022. Selumetinib is a Kinase Inhibitor. The mechanism of action of selumetinib is as a Mitogen-Activated Protein Kinase Kinase 1 Inhibitor, and Mitogen-Activated Protein Kinase Kinase 2 Inhibitor. Selumetinib is an oral, small molecule inhibitor of the mitogen activated protein kinase 1 and 2 (MEK1/2) that is used to treat symptomatic, refractory fibromas in neurofibromatosis type 1. Selumetinib is associated with transient and usually mild elevations in serum aminotransferase levels during therapy, but has not been linked to cases of clinically apparent acute liver injury. Selumetinib is an orally active, small molecule with potential antineoplastic activity. Selumetinib is an ATP-independent inhibitor of mitogen-activated protein kinase kinase (MEK or MAPK/ERK kinase) 1 and 2. MEK 1 and 2 are dual specificity kinases that are essential mediators in the activation of the RAS/RAF/MEK/ERK pathway, are often upregulated in various cancer cells, and are drivers of diverse cellular responses, including proliferation. Inhibition of both MEK1 and 2 by selumetinib prevents the activation of MEK1/2 dependent effector proteins and transcription factors, thereby leading to an inhibition of cellular proliferation in various cancers. See also: Selumetinib Sulfate (has salt form). Drug Indication Selumetinib is indicated for the treatment of neurofibromatosis type 1 (NF1) in patients two years and older who have symptomatic, inoperable plexiform neurofibromas (PN). Koselugo as monotherapy is indicated for the treatment of symptomatic, inoperable plexiform neurofibromas (PN) in paediatric patients with neurofibromatosis type 1 (NF1) aged 3 years and above Treatment of melanoma, Treatment of neurofibromatosis type 1, Treatment of thyroid cancer Mechanism of Action The Ras-Raf-MEK-ERK signaling cascade is known to be activated in several types of cancer, and regulates the transcription of proteins involved in apoptosis. In addition, studies have shown that mutations of the Raf component of the pathway can contribute to chemotherapy drug resistance. Ras as well as several kinases and phosphatases are responsible for regulating the Raf-MEK-ERK pathway. Often in cancers, Ras (a G-protein coupled receptor) is deregulated, allowing downstream signalling to proceed unchecked. Through several complex steps, Raf phosphorylates and activates MEK, which then phosphorylates and activates ERK. ERK is then able to exert its effects on several downstream targets. As such, therapies inhibiting upstream components of this pathway have become attractive targets for cancer treatment. Selumetinib exerts its effects by selectively inhibiting MEK1 and MEK2 which can effectively blunt the pleiotropic effects of the Ras-Raf-MEK-ERK cascade. By inhibiting this oncogenic pathway, selumetinib reduces cell proliferation, and promotes pro-apoptotic signal transduction. |
| Molecular Formula |
C17H15BRCLFN4O3
|
|---|---|
| Molecular Weight |
457.68
|
| Exact Mass |
456
|
| Elemental Analysis |
C, 44.61; H, 3.30; Br, 17.46; Cl, 7.75; F, 4.15; N, 12.24; O, 10.49
|
| CAS # |
606143-52-6
|
| Related CAS # |
Selumetinib sulfate;943332-08-9
|
| PubChem CID |
10127622
|
| Appearance |
white solid powder
|
| Density |
1.7±0.1 g/cm3
|
| Index of Refraction |
1.672
|
| LogP |
5.55
|
| Hydrogen Bond Donor Count |
3
|
| Hydrogen Bond Acceptor Count |
6
|
| Rotatable Bond Count |
6
|
| Heavy Atom Count |
27
|
| Complexity |
523
|
| Defined Atom Stereocenter Count |
0
|
| SMILES |
BrC1C([H])=C([H])C(=C(C=1[H])Cl)N([H])C1=C(C2=C(C([H])=C1C(N([H])OC([H])([H])C([H])([H])O[H])=O)N(C([H])([H])[H])C([H])=N2)F
|
| InChi Key |
CYOHGALHFOKKQC-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C17H15BrClFN4O3/c1-24-8-21-16-13(24)7-10(17(26)23-27-5-4-25)15(14(16)20)22-12-3-2-9(18)6-11(12)19/h2-3,6-8,22,25H,4-5H2,1H3,(H,23,26)
|
| Chemical Name |
6-(4-bromo-2-chloroanilino)-7-fluoro-N-(2-hydroxyethoxy)-3-methylbenzimidazole-5-carboxamide
|
| Synonyms |
selumetinib; ARRY-142886; AZD6244; ARRY142886; ARRY 142886; AZD-6244; AZD 6244; ARRY886; ARRY-886; ARRY 886; 5-[(4-BROMO-2-CHLOROPHENYL)AMINO]-4-FLUORO-N-(2-HYDROXYETHOXY)-1-METHYL-1H-BENZIMIDAZOLE-6-CARBOXAMIDE
|
| HS Tariff Code |
2934.99.9001
|
| Storage |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| Solubility (In Vitro) |
|
|||
|---|---|---|---|---|
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 1 mg/mL (2.18 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution.
For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 10.0 mg/mL clear DMSO stock solution to 400 μL of PEG300 and mix evenly; then add 50 μL of Tween-80 to the above solution and mix evenly; then add 450 μL of normal saline to adjust the volume to 1 mL. Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 1 mg/mL (2.18 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 10.0 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. View More
Solubility in Formulation 3: ≥ 1 mg/mL (2.18 mM) (saturation unknown) in 10% DMSO + 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), clear solution. Solubility in Formulation 4: 4% DMSO+30% PEG 300+5% Tween 80+ddH2O: 5mg/mL |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.1849 mL | 10.9247 mL | 21.8493 mL | |
| 5 mM | 0.4370 mL | 2.1849 mL | 4.3699 mL | |
| 10 mM | 0.2185 mL | 1.0925 mL | 2.1849 mL |
*Note: Please select an appropriate solvent for the preparation of stock solution based on your experiment needs. For most products, DMSO can be used for preparing stock solutions (e.g. 5 mM, 10 mM, or 20 mM concentration); some products with high aqueous solubility may be dissolved in water directly. Solubility information is available at the above Solubility Data section. Once the stock solution is prepared, aliquot it to routine usage volumes and store at -20°C or -80°C. Avoid repeated freeze and thaw cycles.
Calculation results
Working concentration: mg/mL;
Method for preparing DMSO stock solution: mg drug pre-dissolved in μL DMSO (stock solution concentration mg/mL). Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug.
Method for preparing in vivo formulation::Take μL DMSO stock solution, next add μL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O,mix and clarify.
(1) Please be sure that the solution is clear before the addition of next solvent. Dissolution methods like vortex, ultrasound or warming and heat may be used to aid dissolving.
(2) Be sure to add the solvent(s) in order.
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT03326310 | Recruiting | Drug: Azacitidine Drug: Selumetinib |
Chronic Myeloid Leukemia Myelofibroses |
University of Chicago | September 4, 2018 | Phase 1 |
| NCT04924608 | Active Recruiting |
Drug: Selumetinib Other: Placebo |
Neurofibromatosis 1 Plexiform Neurofibroma (PN) |
AstraZeneca | November 19, 2021 | Phase 3 |
| NCT04590235 | Active Recruiting |
Drug: Selumetinib | Neurofibromatosis 1 Neurofibroma Plexiform |
AstraZeneca | December 16, 2020 | Phase 1 |
| NCT05101148 | Active Recruiting |
Drug: Selumetinib | Neurofibromatosis Type 1 | AstraZeneca | July 21, 2021 | Phase 1 |
| NCT03095248 | Recruiting | Drug: Selumetinib | Glioma Meningioma |
Children's Hospital Medical Center, Cincinnati |
May 8, 2017 | Phase 2 |
Structure of ARRY-142886 and its ability to inhibit enzymatic MEK1 activity.Clin Cancer Res.2007 Mar 1;13(5):1576-83. |
Inhibition of tumor growth and decreased tumor phospho-ERK1/2 levels in a mouse HT-29 xenograft model.
Inhibition of basal and induced ERK1/2 phosphorylation in human cancer cell lines and PBMCs.Clin Cancer Res.2007 Mar 1;13(5):1576-83. |
Tumor growth inhibition in the mouse BxPC3 xenograft model.Clin Cancer Res.2007 Mar 1;13(5):1576-83. |
 |
 |