
| Size | Price | Stock | Qty |
|---|---|---|---|
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|
Purity: ≥98%
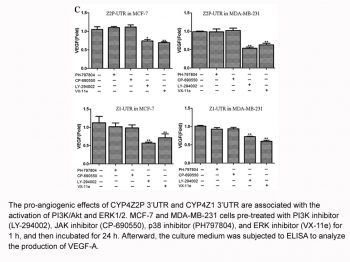
Tofacitinib (also known as tasocitinib or CP-690550, sold under the brand Xeljanz), is a novel and potent inhibitor of JAK3 (Janus-Associated kinase) with potential anti-inflammatory activity. It inhibits JAK1, JAK2, and JAK3 with IC50s of 1.0 nM, 21.7 nM, and 6.5 nM, respectively, in cell-free assays. It is an FDA approved drug for the treatment of rheumatoid arthritis (RA), psoriatic arthritis, and ulcerative colitis. The inhibition is JAK3-specific with a selectivity of 1000-fold higher than other non-JAK family kinases.
| Targets |
JAK3 (IC50 = 1 nM); JAK2 (IC50 = 20 nM); JAK1 (IC50 = 112 nM); Rock-II (IC50 = 3400 nM); Lck (IC50 = 3870 nM)
|
||
|---|---|---|---|
| ln Vitro |
JAK3 and JAK2 may bind to tofacitinib (CP-690550) Citrate at 2.2 nM and 5 nM (Kd) concentrations. In Camk1 (Kd 5,000 nM), DCamkL3 (Kd 4.5 nM), Mst2 (Kd 4,300 nM), Pkn1 (Kd 200 nM), and Rps6ka2 (Kin.Dom.2-C-), tofacitinib is included in the report. Kd 1,400 nM for the terminal), Kd 1,200 nM for Rps6ka6 (Kin.Dom.2-C terminal), Kd 420 nM for Snark, Kd 640 nM for Tnk1, and Kd 620 nM for Tyk2][1].
|
||
| ln Vivo |
For five weeks following their initial immunization (p<0.01, n=8), animals treated with tofacitinib exhibit a considerably decreased development of anti-drug antibodies (ADAs) when compared to PEG-treated control mice. Additionally, day 28 is when ADAs become noticeable. Titers to SS1P show a 1000- to 200-fold variation from days 21 to 35, respectively. Keyhole limpet hemocyanin (KLH)-injected animals produce an antibody response more quickly than those treated with SS1P. Nevertheless, tofacitinib dosing lowers anti-KLH titers in comparison to controls (p<0.05 on day 21 and p<0.01 on day 28, respectively, n = 5). From days 21 through 28, titer reductions varied from 5000 to 250 fold[2]. The JAK1 and JAK3 signaling pathways can be suppressed for more than 4 hours with a daily dose of tofacitinib of 6.2 mg/kg, which is chosen based on prior dose-response experiments and provides 80% inhibition of hind paw volume and plasma exposure[3].
Tofacitinib by oral route inhibited the LPS-induced airway neutrophilia, the levels of some cytokines in the BALF and the phosphorylation of STAT3 in the lung tissue. Conclusions and implications: In summary, this study shows that JAK inhibition ameliorates inhaled LPS-induced airway inflammation in rats, suggesting that at least JAK/STAT3 signalling is involved in the establishment of the pulmonary neutrophilia induced by LPS. JAKs inhibitors should be further investigated as a potential therapy for respiratory inflammatory diseases.[4] Immunogenicity remains the "Achilles' heel" of protein-based therapeutics. Anti-drug Abs produced in response to protein therapeutics can severely limit both the safety and efficacy of this expanding class of agent. In this article, we report that monotherapy of mice with tofacitinib (the JAK inhibitor) quells Ab responses to an immunotoxin derived from the bacterial protein Pseudomonas exotoxin A, as well as to the model Ag keyhole limpet hemocyanin. Thousand-fold reductions in IgG1 titers to both Ags were observed 21 d post immunization. In fact, suppression was evident for all IgG isotypes and IgM. A reduction in IgG3 production was also noted with a thymus-independent type II Ag. Mechanistic investigations revealed that tofacitinib treatment led to reduced numbers of CD127+ pro-B cells. Furthermore, we observed fewer germinal center B cells and the impaired formation of germinal centers of mice treated with tofacitinib. Because normal Ig levels were still present during tofacitinib treatment, this agent specifically reduced anti-drug Abs, thus preserving the potential efficacy of biological therapeutics, including those used as cancer therapeutics[2]. |
||
| Enzyme Assay |
Kinase profiles were performed by a CRO utilizing KINOMEscan™. Activity is recorded via a competition binding assay of selected kinases that are fused to a proprietary tag. Measurements of the amount of kinase bound to an immobilized, active-site directed ligand in the presence and absence of the test compound provide a % of DMSO control for binding of ligand. Activities between 0 and 10 were selected for Kd determinations. Dendrogram representations were generated by an in-house visualization tool designated PhyloChem. Dendrogram clustering and apexes are based on the human phylogenetic kinase data available at http://kinase.com/human/kinome[1].
|
||
| Cell Assay |
Characterization of B cell differentiation and proliferation[2]
Splenocyte and bone marrow cell suspensions were prepared from BALB/c mice and total cells were counted. Cells (1×106) were stained with various combinations of the following anti-murine antibodies): CD3, B220, CD43, IgM, Fas, GL-7, CD24, BP-1, CD127 or IgG1-conjugated with FITC, PE or APC and analyzed on a FACSCalibur flow cytometer. At least 10,000 live events were acquired. For assessment of in vitro B cell proliferation CD43- splenocytes were MACS purified and labeled with 1 μM CFSE according to the manufacturer’s instructions. Labeled cells were activated for 48 hours with 25 μg/mL LPS (Escherichia coli 0111:B4) and 5 ng/ml IL-4 in the presence of 0, 0.1, 0.3, or 1.0 μM tofacitinib. Following culture, cells were washed, surface stained and examined by flow cytometry. In vitro human osteoclast differentiation and function.[3] Primary human monocytes were obtained by negative selection of CD14+ cells from leukopaks using magnetic-activated cell sorting (MACS) cell separation technology. Cells were plated in 96-well black tissue culture plates at 1 × 105 cells/well in high-glucose Dulbecco's modified Eagle's medium containing 5% fetal bovine serum (FBS) and 10 units/ml penicillin–streptomycin. Cultured cells were treated every other day for 14 days with either 25 ng/ml recombinant human macrophage colony-stimulating factor (M-CSF) for macrophage differentiation, or M-CSF in the presence of 100 ng/ml of recombinant human RANKL for osteoclast differentiation. Cells were also treated with or without varying concentrations of tofacitinib in 0.2% DMSO at the same time as differentiating cytokines. TRAP activity was quantified using ELF-97 fluorescent phosphatase substrate. Cells were then fixed and stained using a Leukocyte Acid Phosphatase kit according to the recommendations of the manufacturer.[3] Functional bone resorptive activity of human osteoclasts was measured by OsteoLyse assay. Human osteoclast precursor cells (Lonza) were plated at 1 × 104 cells/well in medium containing 33 ng/ml M-CSF and 66 ng/ml RANKL on 96-well OsteoLyse cell culture plates precoated with europium-conjugated human type I collagen. During the differentiation phase (days 0–6), cells were treated with varying concentrations of tofacitinib or left untreated. After 6 days in culture, fresh medium containing M-CSF and RANKL was added, and tofacitinib was replaced at the same concentrations or added to previously untreated cells. Additionally, alendronate sodium was added to untreated cells as a positive control. Cells were cultured for an additional 4 days to allow collagen release by functionally active osteoclasts, and culture supernatants were assayed for europium fluorescence using OsteoLyse Fluorophore-Releasing Reagent with measurement of time-resolved fluorescence over a 400 μsec interval at 340 nm excitation and 615 nm emission. In vitro human T lymphocyte RANKL production.[3] CD4+ T lymphocytes were negatively selected from a leukopak using MACS cell separation technology and cultured at 2.5 × 105 cells/well in round-bottomed 96-well tissue culture plates in RPMI 1640 medium containing glucose, 10% FBS, and 10 units/ml penicillin–streptomycin. Cells were treated with or without varying concentrations of tofacitinib in 0.2% DMSO and activated for 5 days with 1 μg/ml anti-human CD3 and 0.1 μg/ml anti-human CD28 antibodies together with 50 ng/ml recombinant human IL-2. RANKL secreted into culture medium was measured using a human LincoPlex assay. |
||
| Animal Protocol |
|
||
| ADME/Pharmacokinetics |
Absorption, Distribution and Excretion
74% oral absorption (absolute bioavailability), with peak plasma concentrations (T max) achieved in 0.5-1 hour. Administration with fatty meals does not alter AUC but reduces Cmax by 32%. 70% metabolized in the liver by CYP3A4 (major) and CYP2C19 (minor). Metabolites produced are inactive. 30% renally eliminated as unchanged drug. Vd= 87L after intravenous administration. Distribution is equal between red blood cells and plasma. The protein binding of tofacitinib is approximately 40%. Tofacitinib binds predominantly to albumin and does not appear to bind to a1-acid glycoprotein. Tofacitinib distributes equally between red blood cells and plasma. The absolute oral bioavailability of tofacitinib is 74%. Coadministration of Xeljanz with a high-fat meal resulted in no changes in AUC while Cmax was reduced by 32%. In clinical trials, Xeljanz was administered without regard to meals. Clearance mechanisms for tofacitinib are approximately 70% hepatic metabolism and 30% renal excretion of the parent drug. The metabolism of tofacitinib is primarily mediated by CYP3A4 with minor contribution from CYP2C19. In a human radiolabeled study, more than 65% of the total circulating radioactivity was accounted for by unchanged tofacitinib, with the remaining 35% attributed to 8 metabolites, each accounting for less than 8% of total radioactivity. The pharmacologic activity of tofacitinib is attributed to the parent molecule. Following oral administration of Xeljanz /to humans/, peak plasma concentrations are reached within 0.5-1 hour, elimination half-life is approximately 3 hours and a dose-proportional increase in systemic exposure was observed in the therapeutic dose range. Steady state concentrations are achieved in 24-48 hours with negligible accumulation after twice daily administration. /MILK/ Tofacitinib was secreted in milk of lactating rats. It is not known whether tofacitinib is excreted in human milk. Metabolism / Metabolites Metabolized in the liver by CYP3A4 and CYP2C19. Metabolites produced are inactive. Clearance mechanisms for tofacitinib are approximately 70% hepatic metabolism and 30% renal excretion of the parent drug. The metabolism of tofacitinib is primarily mediated by CYP3A4 with minor contribution from CYP2C19. In a human radiolabeled study, more than 65% of the total circulating radioactivity was accounted for by unchanged tofacitinib, with the remaining 35% attributed to 8 metabolites, each accounting for less than 8% of total radioactivity. The pharmacologic activity of tofacitinib is attributed to the parent molecule. Biological Half-Life ~3 hours The elimination half-life of tofacitinib /in humans/ is approximately 3 hours. |
||
| Toxicity/Toxicokinetics |
Toxicity Summary
IDENTIFICATION AND USE: Tofacitinib is a yellow foam. As the drug Xeljanz, it is indicated for the treatment of adult patients with moderately to severely active rheumatoid arthritis (RA) who have had an inadequate response or intolerance to methotrexate. It may be used as monotherapy or in combination with methotrexate or other nonbiologic disease-modifying antirheumatic drugs (DMARDs). HUMAN EXPOSURE AND TOXICITY: According to epidemiological studies, the overall risk of infection (including serious infection) and mortality rates in RA patients treated with tofacitinib appear to be similar to those observed in RA patients treated with biologic agents. The rates of serious infection were stable over time. Within the global tofacitinib RA development program, tuberculosis was the most common opportunistic infection reported but was rare in regions of low and medium TB incidence. In a genotoxicity study, increases in chromosomal abnormalities were observed in a human lymphocyte in vitro cytogenetic assay, at high cytotoxic concentrations with metabolic activation, but no effects were observed without metabolic activation. ANIMAL STUDIES: In cynomolgus monkeys, emesis and decreased activity were observed as a result of acute exposure. Xeljanz caused death in rats at single oral doses of >/= 500 mg/kg. Immune and hematopoietic organ systems were identified as main targets in repeat-dose toxicity studies on animals. In a peri/postnatal development study in rats, Xeljanz decreased the number of delivered and live born pups, and reduced pup survival at oral doses of 50 mg/kg/day. Xeljanz was teratogenic (external, visceral and skeletal abnormalities) in rabbits and rats at oral doses of 30 and 100 mg/kg/day, respectively. Xeljanz was not mutagenic in the bacterial reverse mutation assay. Xeljanz was not mutagenic in mammalian cells (in vitro CHO/HGPRT assay) and did not induce primary DNA damage in an in vivo/in vitro rat hepatocyte unscheduled DNA synthesis assay. Xeljanz was also negative in the in vivo rat micronucleus test. In a 2-year rat carcinogenicity study, Xeljanz induced benign Leydig cell tumors and malignant hibernomas at oral doses of >/= 30 mg/kg/day and benign thymomas at 100/75 mg/kg/day. In a 39-week repeat-dose toxicity study in adult monkeys, lymphomas were observed at the high dose of 5 mg/kg twice daily, but not at the lower dose of 1 mg/kg twice daily (approximately equivalent to human exposure). Interactions In healthy individuals, the CYP3A inducer rifampin (600 mg orally once daily for 7 days) decreased peak plasma concentrations and AUC of tofacitinib (single oral dose of 30 mg) by 74 and 84%, respectively. Concomitant use of rifampin may decrease efficacy of tofacitinib. There is a risk of added immunosuppression when Xeljanz is coadministered with potent immunosuppressive drugs (e.g., azathioprine, tacrolimus, cyclosporine). Combined use of multiple-dose Xeljanz with potent immunosuppressants has not been studied in rheumatoid arthritis. Use of Xeljanz in combination with biologic disease-modifying antirheumatic drugs (DMARDS) or potent immunosuppressants such as azathioprine and cyclosporine is not recommended. Concomitant use of tofacitinib with potent immunosuppressive agents (e.g., azathioprine, cyclosporine, tacrolimus) increases the risk of immunosuppression and is not recommended. Concomitant use of tofacitinib with such agents in patients with rheumatoid arthritis has not been studied to date. In healthy individuals, cyclosporine (200 mg orally every 12 hours for 5 days) decreased the clearance of tofacitinib (single oral dose of 10 mg), resulting in a 73% increase in the AUC of tofacitinib, accompanied by a 17% decrease in peak plasma tofacitinib concentrations. In healthy individuals, tacrolimus (5 mg orally every 12 hours for 7 days) slightly decreased the clearance of tofacitinib (single oral dose of 10 mg), resulting in a 21% increase in the AUC of tofacitinib, accompanied by a 9% decrease in peak plasma tofacitinib concentrations. Tofacitinib exposure is decreased when Xeljanz is coadministered with potent CYP3A4 inducers (e.g., rifampin). For more Interactions (Complete) data for Tofacitinib (9 total), please visit the HSDB record page. |
||
| References |
|
||
| Additional Infomation |
Therapeutic Uses
Protein Kinase Inhibitors /CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Tofacitinib is included in the database. Xeljanz (tofacitinib) is indicated for the treatment of adult patients with moderately to severely active rheumatoid arthritis who have had an inadequate response or intolerance to methotrexate. It may be used as monotherapy or in combination with methotrexate or other nonbiologic disease-modifying antirheumatic drugs (DMARDs). /Included in US product label/ EXPL Tofacitinib is an oral Janus kinase inhibitor that is being investigated for psoriasis and psoriatic arthritis. Japanese patients aged 20 years or more with moderate to severe plaque psoriasis and/or psoriatic arthritis were double-blindly randomized 1:1 to tofacitinib 5 or 10 mg b.i.d. for 16 weeks, open-label 10 mg b.i.d. for 4 weeks, then variable 5 or 10 mg b.i.d. to Week 52. Primary end-points at Week 16 were the proportion of patients achieving at least a 75% reduction in Psoriasis Area and Severity Index (PASI75) and Physician's Global Assessment of "clear" or "almost clear" (PGA response) for psoriasis, and 20% or more improvement in American College of Rheumatology criteria (ACR20) for patients with psoriatic arthritis. Safety was assessed throughout. Eighty-seven patients met eligibility criteria for moderate to severe plaque psoriasis (5 mg b.i.d., n = 43; 10 mg b.i.d., n = 44), 12 met eligibility criteria for psoriatic arthritis (5 mg b.i.d., n = 4; 10 mg b.i.d., n = 8) including five who met both criteria (10 mg b.i.d.). At Week 16, 62.8% and 72.7% of patients achieved PASI75 with tofacitinib 5 and 10 mg b.i.d., respectively; 67.4% and 68.2% achieved PGA responses; all patients with psoriatic arthritis achieved ACR20. Responses were maintained through Week 52. Adverse events occurred in 83% of patients through Week 52, including four (4.3%) serious adverse events and three (3.2%) serious infections (all herpes zoster). No malignancies, cardiovascular events or deaths occurred. Tofacitinib (both doses) demonstrated efficacy in patients with moderate to severe plaque psoriasis and/or psoriatic arthritis through 52 weeks; safety findings were generally consistent with prior studies. EXPL The inflammatory diseases ulcerative colitis and Crohn's disease constitute the two main forms of inflammatory bowel disease (IBD). They are characterized by chronic, relapsing inflammation of the gastrointestinal tract, significantly impacting on patient quality of life and often requiring prolonged treatment. Existing therapies for IBD are not effective for all patients, and an unmet need exists for additional therapies to induce and maintain remission. Here we describe the mechanism of action of the Janus kinase (JAK) inhibitor, tofacitinib, for the treatment of IBD and the effect of JAK inhibition on the chronic cycle of inflammation that is characteristic of the disease. The pathogenesis of IBD involves a dysfunctional response from the innate and adaptive immune system, resulting in overexpression of multiple inflammatory cytokines, many of which signal through JAKs. Thus JAK inhibition allows multiple cytokine signaling pathways to be targeted and is expected to modulate the innate and adaptive immune response in IBD, thereby interrupting the cycle of inflammation. Tofacitinib is an oral, small molecule JAK inhibitor that is being investigated as a targeted immunomodulator for IBD. Clinical development of tofacitinib and other JAK inhibitors is ongoing, with the aspiration of providing new treatment options for IBD that have the potential to deliver prolonged efficacy and clinically meaningful patient benefits. Drug Warnings /BOXED WARNING/ WARNING: SERIOUS INFECTIONS. Patients treated with Xeljanz are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids. If a serious infection develops, interrupt Xeljanz until the infection is controlled. Reported infections include: Active tuberculosis, which may present with pulmonary or extrapulmonary disease. Patients should be tested for latent tuberculosis before Xeljanz use and during therapy. Treatment for latent infection should be initiated prior to Xeljanz use. Invasive fungal infections, including cryptococcosis and pneumocystosis. Patients with invasive fungal infections may present with disseminated, rather than localized, disease. Bacterial, viral, and other infections due to opportunistic pathogens. The risks and benefits of treatment with Xeljanz should be carefully considered prior to initiating therapy in patients with chronic or recurrent infection. Patients should be closely monitored for the development of signs and symptoms of infection during and after treatment with Xeljanz, including the possible development of tuberculosis in patients who tested negative for latent tuberculosis infection prior to initiating therapy /BOXED WARNING/ MALIGNANCIES. Lymphoma and other malignancies have been observed in patients treated with Xeljanz. Epstein Barr Virus-associated post-transplant lymphoproliferative disorder has been observed at an increased rate in renal transplant patients treated with Xeljanz and concomitant immunosuppressive medications Patients receiving tofacitinib are at increased risk of developing serious infections that may require hospitalization or result in death. Opportunistic infections caused by bacterial, mycobacterial, invasive fungal, viral, or other opportunistic organisms-including cryptococcosis, pneumocystosis, tuberculosis and other mycobacterial infections, esophageal candidiasis, multidermatomal herpes zoster, cytomegalovirus infection, and BK virus infection-have been reported in patients with rheumatoid arthritis receiving tofacitinib. Patients with invasive fungal infections may present with disseminated, rather than localized, disease. Patients should be closely monitored during and after treatment with tofacitinib for the development of signs or symptoms of infection (e.g., fever, malaise, weight loss, sweats, cough, dyspnea, pulmonary infiltrates, serious systemic illness including shock). Most patients who developed serious infections were receiving concomitant therapy with immunosuppressive agents such as methotrexate or corticosteroids. Tofacitinib therapy should not be initiated in patients with active infections, including localized infections. Tofacitinib should be discontinued in patients who develop a serious infection, opportunistic infection, or sepsis and should not be resumed until the infection is controlled. Clinicians should consider potential risks and benefits of tofacitinib prior to initiating therapy in patients with a history of chronic, recurring, serious, or opportunistic infections; patients with underlying conditions that may predispose them to infections; and patients who have been exposed to tuberculosis or who reside or have traveled in regions where tuberculosis or mycoses are endemic. Any patient who develops a new infection while receiving tofacitinib should undergo a thorough diagnostic evaluation (appropriate for an immunocompromised patient), appropriate anti-infective therapy should be initiated, and the patient should be closely monitored. For more Drug Warnings (Complete) data for Tofacitinib (22 total), please visit the HSDB record page. Pharmacodynamics Tofacitinib targets inflammation present in rheumatoid arthritis by inhibiting the janus kinases involved in the inflammatory response pathway. In placebo controlled trials of rheumatoid arthritis patients receiving 5mg or 10mg of tofacitinib twice daily, higher ACR20 responses were observed within 2 weeks in some patients (with ACR20 being defined as a minimum 20% reduction in joint pain or tenderness and 20% reduction in arthritis pain, patient disability, inflammatory markers, or global assessments of arthritis by patients or by doctors, according to the American College of Rheumatology (ACR) response criteria list), and improvements in physical functioning greater than placebo were also noted. Common known adverse effects of tofacitinib include headaches, diarrhea, nausea, nasopharyngitis and upper respiratory tract infection. More serious immunologic and hematological adverse effects have also been noted resulting in lymphopenia, neutropenia, anemia, and increased risk of cancer and infection. Before initiations of tofacitinib patients should be tested for latent infections of tuberculosis, and should be closely monitored for signs and symptoms of infection (fungal, viral, bacterial, or mycobacterial) during therapy. Therapy is not to be started in the presence of active infection, systemic or localized, and is to be interrupted if a serious infection occurs. Tofacitinib has been associated with an increased risk of lymphomas, such as Epstein-Barr virus associated lymphomas, and other malignancies (including lung, breast, gastric, and colorectal cancers). It is recommended to monitor lymphocytes, neutrophils, hemoglobin, liver enzymes, and lipids. Tofacitinib use is associated with a rapid decrease in C-reactive protein (CRP), dose dependent decreases in natural killer cells, and dose dependent increases in B cells. Depression in C-reactive protein levels continue after 2 weeks of tofacitinib discontinuation and suggest that pharmacodynamic activity last longer than pharmacokinetic half life. |
| Molecular Formula |
C16H20N6O
|
|---|---|
| Molecular Weight |
312.37
|
| Exact Mass |
312.169
|
| Elemental Analysis |
C, 61.52; H, 6.45; N, 26.90; O, 5.12
|
| CAS # |
477600-75-2
|
| Related CAS # |
Tofacitinib citrate;540737-29-9;(3S,4S)-Tofacitinib;1092578-47-6;(3R,4S)-Tofacitinib;1092578-46-5;(3S,4R)-Tofacitinib;1092578-48-7;Tofacitinib-13C3; 1443435-54-8 (oxalate); 477600-75-2; 1803005-18-6 (HCl); 1443435-50-4 (tartrate); 2052885-67-1; 1803005-19-7 (HBr)
|
| PubChem CID |
9926791
|
| Appearance |
Off-white to light yellow solid powder
|
| Density |
1.3±0.1 g/cm3
|
| Boiling Point |
585.8±50.0 °C at 760 mmHg
|
| Melting Point |
White crystalline solid. MP: 199-206 °C /Tofacitinib monocitrate/
|
| Flash Point |
308.1±30.1 °C
|
| Vapour Pressure |
0.0±1.6 mmHg at 25°C
|
| Index of Refraction |
1.646
|
| LogP |
0.93
|
| Hydrogen Bond Donor Count |
1
|
| Hydrogen Bond Acceptor Count |
5
|
| Rotatable Bond Count |
3
|
| Heavy Atom Count |
23
|
| Complexity |
488
|
| Defined Atom Stereocenter Count |
2
|
| SMILES |
C[C@@H]1CCN(C[C@@H]1N(C)C2=NC=NC3=C2C=CN3)C(=O)CC#N
|
| InChi Key |
UJLAWZDWDVHWOW-YPMHNXCESA-N
|
| InChi Code |
InChI=1S/C16H20N6O/c1-11-5-8-22(14(23)3-6-17)9-13(11)21(2)16-12-4-7-18-15(12)19-10-20-16/h4,7,10-11,13H,3,5,8-9H2,1-2H3,(H,18,19,20)/t11-,13+/m1/s1
|
| Chemical Name |
3-((3R,4R)-4-Methyl-3-(methyl(7H-pyrrolo[2,3-d]pyrimidin-4-yl)amino)piperidin-1-yl)-3-oxopropanenitrile
|
| Synonyms |
CP-690550; CP690550; CP 690550; Tasocitinib; Tasocitinib; 3-((3R,4R)-4-methyl-3-(methyl(7H-pyrrolo[2,3-d]pyrimidin-4-yl)amino)piperidin-1-yl)-3-oxopropanenitrile; CP-690550; CP 690550; 1259404-17-5; rac-Tofacitinib; Tofacitinib; Xeljanz (Trade name); Tofacitinib free base;
|
| HS Tariff Code |
2934.99.9001
|
| Storage |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| Shipping Condition |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| Solubility (In Vitro) |
|
|||
|---|---|---|---|---|
| Solubility (In Vivo) |
Solubility in Formulation 1: ≥ 2.5 mg/mL (8.00 mM) (saturation unknown) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution.
Preparation of saline: Dissolve 0.9 g of sodium chloride in 100 mL ddH₂ O to obtain a clear solution. Solubility in Formulation 2: ≥ 2.5 mg/mL (8.00 mM) (saturation unknown) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. View More
Solubility in Formulation 3: ≥ 2.08 mg/mL (6.66 mM) (saturation unknown) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (add these co-solvents sequentially from left to right, and one by one), clear solution. Solubility in Formulation 4: ≥ 2.08 mg/mL (6.66 mM) (saturation unknown) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 20.8 mg/mL clear DMSO stock solution to 900 μL of 20% SBE-β-CD physiological saline solution and mix evenly. Preparation of 20% SBE-β-CD in Saline (4°C,1 week): Dissolve 2 g SBE-β-CD in 10 mL saline to obtain a clear solution. Solubility in Formulation 5: ≥ 2.08 mg/mL (6.66 mM) (saturation unknown) in 10% DMSO + 90% Corn Oil (add these co-solvents sequentially from left to right, and one by one), clear solution. For example, if 1 mL of working solution is to be prepared, you can add 100 μL of 20.8 mg/mL clear DMSO stock solution to 900 μL of corn oil and mix evenly. Solubility in Formulation 6: 30% PEG400+0.5% Tween80+5% propylene glycol:30mg/mL Solubility in Formulation 7: 5 mg/mL (16.01 mM) in 0.5% MC 0.5% Tween-80 (add these co-solvents sequentially from left to right, and one by one), suspension solution; with ultrasonication. |
| Preparing Stock Solutions | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.2013 mL | 16.0067 mL | 32.0133 mL | |
| 5 mM | 0.6403 mL | 3.2013 mL | 6.4027 mL | |
| 10 mM | 0.3201 mL | 1.6007 mL | 3.2013 mL |
*Note: Please select an appropriate solvent for the preparation of stock solution based on your experiment needs. For most products, DMSO can be used for preparing stock solutions (e.g. 5 mM, 10 mM, or 20 mM concentration); some products with high aqueous solubility may be dissolved in water directly. Solubility information is available at the above Solubility Data section. Once the stock solution is prepared, aliquot it to routine usage volumes and store at -20°C or -80°C. Avoid repeated freeze and thaw cycles.
Calculation results
Working concentration: mg/mL;
Method for preparing DMSO stock solution: mg drug pre-dissolved in μL DMSO (stock solution concentration mg/mL). Please contact us first if the concentration exceeds the DMSO solubility of the batch of drug.
Method for preparing in vivo formulation::Take μL DMSO stock solution, next add μL PEG300, mix and clarify, next addμL Tween 80, mix and clarify, next add μL ddH2O,mix and clarify.
(1) Please be sure that the solution is clear before the addition of next solvent. Dissolution methods like vortex, ultrasound or warming and heat may be used to aid dissolving.
(2) Be sure to add the solvent(s) in order.
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT06202560 | Enrolling by invitation | Drug: Tofacitinib 5 MG | Frontal Fibrosing Alopecia Lichen Planopilaris |
Institute of Dermatology, Thailand | November 29, 2023 | Not Applicable |
| NCT06044844 | Recruiting | Drug: Tofacitinib | Efficacy of Tofacitinib in the Systemic Sclerosis |
Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh |
November 2023 | Phase 2 |
| NCT04424303 | Recruiting | Drug: Tofacitinib | Ulcerative Colitis | Pfizer | December 4, 2020 | |
| NCT06278402 | Completed | Drug: Tofacitinib | Alopecia Areata Alopecia Totalis |
Jinnah Hospital | July 1, 2023 | Phase 3 |
 |
|
 |